Antibiotic Guidelines

Antibiotic Guidelines
Infection Management Guidelines Empirical Antibiotic Therapy in Adults
- STOP AND THINK BEFORE ANTIBIOTIC THERAPY: 1 in 5 antibiotic courses associated with adverse events, including C.difficile, drug interactions/ toxicity, device-related infections and S. aureus bacteraemia.
- THINK SEPSIS if NEWS ≥ 5. Send samples to microbiology before starting antibiotics.
- RECORD antibiotic indication.
- REVIEW patients and results.
- RECORD clinical response and prescription daily.
- Can you SIMPLIFY, SWITCH or STOP?
- If Clinical improvement + eating/drinking + deep seated/complex infection not suspected.
- IVOST and RECORD duration of remaining oral therapy.
- RECORD the STOP date for oral antibiotics – score the appropriate date.
- REVIEW all IV antibiotics DAILY and RECORD review date.
- INFORM patient of the reason for the antibiotic and likely duration.
Definition of SEPSIS:
- INFECTION (includes Systemic Inflammatory Response Syndrome (SIRS*).
- WITH evidence of ORGAN HYPOPERFUSION (≥ 2 of Confusion, < 15 GCS or Resp Rate ≥ 22/ min or Systolic BP ≤ 100 mm Hg).
- Ensure SEPSIS 6 within one hour:
- Blood cultures (& any other relevant samples)
- IV Antibiotic administration
- Oxygen to maintain target saturation
- Measure lactate,
- IV fluids,
- Monitor urine output hourly.
- *SIRS indicated by Temp < 36°C or > 38°C, HR > 90 bpm, RR> 20/ min & WCC < 4 or > 12 x109/ L.
- The SIRS is not specific to bacterial infection (also viral & non-infective causes).

Infective Exacerbation COPD and Antibiotic Guidelines
- Only if purulent sputum (send for culture along with viral gargle)
- Dual antibiotic therapy is not recommended & increases the risk of harm
- Oral ▲Doxycycline 200mg as a one-off single dose then 100mg daily or Oral Amoxicillin 500mg 8 hourly or Oral ■ Clarithromycin 500mg 12 hourly
- Duration 5 days
Highly recommend to subscribe in GetResponseGetResponse

Suspected COVID-19 pneumonia
- Antibiotics NOT usually required
- Antibiotics only if COPD with purulent sputum (treat as above) or suspected bacterial pneumonia with Chest X-Ray changes (treat as Pneumonia below)
- Consider stopping antibiotics following review and positive SARS-CoV-2 result
Uncertain if LRTI/ UTI
- Send MSSU, sputum and viral gargle
- Oral Co-trimoxazole 960mg 12 hourly or Oral ▲Doxycycline 100mg 12 hourly
- Do NOT prescribe Co-amoxiclav
- Review/ clarify diagnosis at 48 hours
- Duration if a diagnosis remains uncertain MAXIMUM 5 days
Pneumonia – Community-Acquired Pneumonia (CAP)
- Assess for SEPSIS
- Calculate CURB 65 score:
- Confusion (new onset)
- Urea > 7 mmol/L
- RR ≥ 30 breaths/ min
- BP – diastolic ≤ 60 mmHg or systolic < 90 mmHg
- Age ≥ 65 years
Non-severe CAP
- CURB 65 score: ≤ 2 (and no sepsis)
- Oral Amoxicillin 500mg 8 hourly or Oral ▲Doxycycline 200mg as a one-off single dose then 100mg daily or Oral ■ Clarithromycin 500mg 12 hourly
- Duration 5 days
Severe CAP
- CURB 65 score ≥ 3 or CAP (with any CURB 65 score) PLUS sepsis syndrome:
- IV/oral ■ Clarithromycin 500mg 12 hourly PLUS either: IV Amoxicillin 1g 8 hrly or if requiring HDU/ ICU level care
- IV Co-amoxiclav 1.2g 8 hrly
- If true penicillin/beta-lactam allergy or Legionella strongly suspected
- Oral/IV ■ Levofloxacin 500mg 12 hourly monotherapy (NB oral bioavailability 99 – 100 %)
- Duration 5 days (IV/oral)
- Legionella 10-14 days
Hospital Acquired Pneumonia (HAP)
- Diagnosis of HAP is complex, and it is often over-diagnosed. Consider other causes of clinical deterioration, including hospital-onset COVID-19, and review diagnosis early.
- Seek senior advice. Assess severity based on the CURB 65 score.
- If within four days of admission. Treat as for CAP
- If ≤ 7 days post-hospital discharge or ≥ 5 days after admission:
Non-severe HAP
- Oral therapy recommended
- Oral ▲Doxycycline 100mg 12 hourly
- or Oral Co-trimoxazole 960mg 12 hourly
- Duration 5 days
Severe HAP
- IV Co-trimoxazole 960mg 12 hourly (or if allergy IV Co-amoxiclav 1.2g 8 hrly) + IV Gentamicin**∆ (max 4 days)
- See BNF for dosing of co-trimoxazole in renal impairment if eGFR < 20 mL/min/ 1.73 m2 contact infection specialist
- Duration 5 days (IV/oral)
- If critically ill, discuss with an infection specialist
Aspiration pneumonia
- This is a chemical injury and does not indicate antibiotic treatment.
- Reserve antibiotics for those who fail to improve within 48 hrs post aspiration.
- IV Amoxicillin 1g 8 hrly or if true penicillin/beta-lactam allergy
- IV ■ Clarithromycin 500mg 12 hourly + IV Metronidazole 500mg 8 hourly
- Duration 5 days (IV/oral)
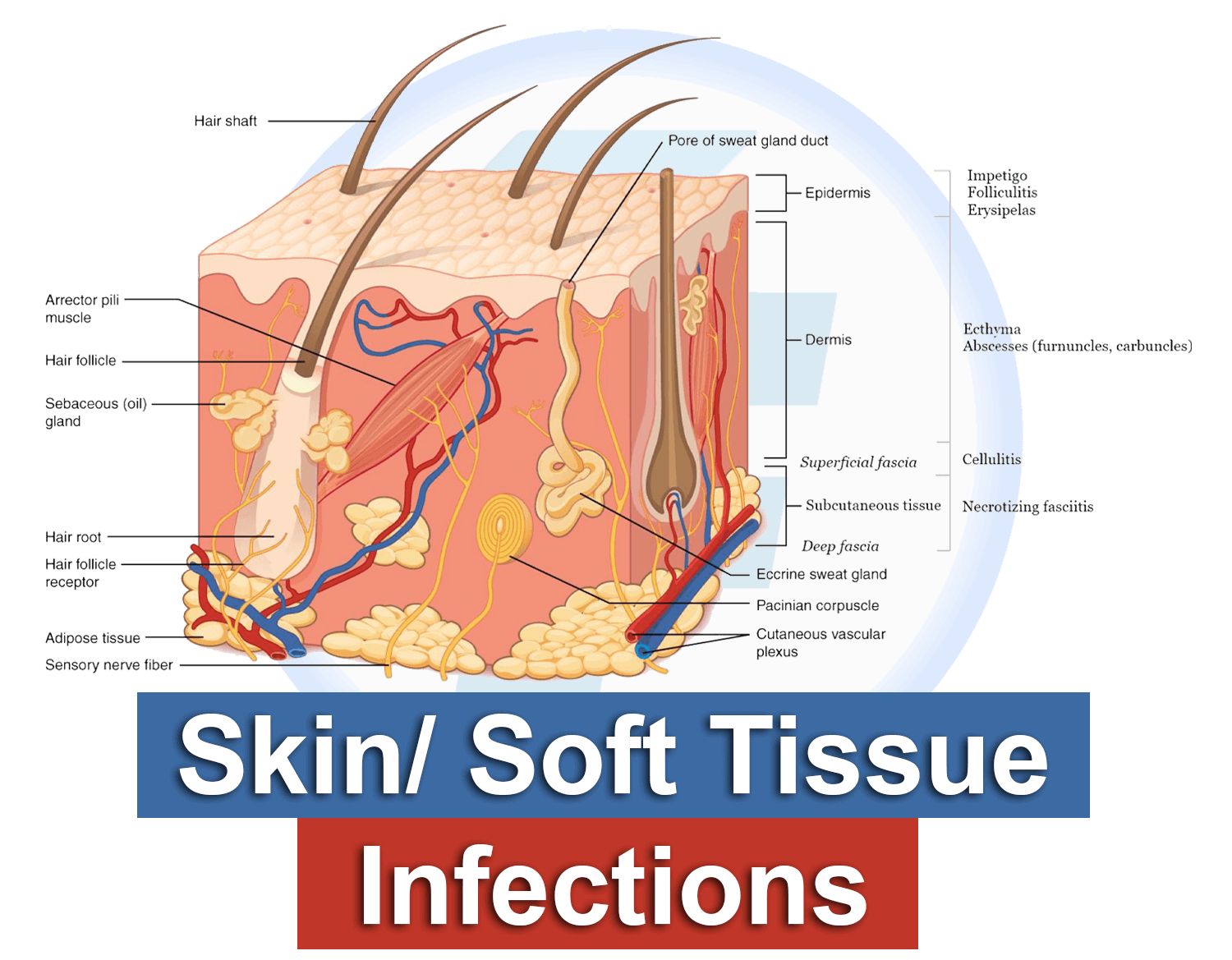
Mild skin/soft tissue infection
- Oral Flucloxacillin 1g 6 hrly or if true penicillin/beta-lactam allergy
- Oral Co-trimoxazole 960mg 12 hourly or Oral ▲Doxycycline 100mg 12 hourly
- Duration 5 days
Moderate / Severe Cellulitis
- Consider OPAT/ ambulatory care (consult local management pathway).
- If requires inpatient management: IV Flucloxacillin 2g 6 hrly
- If MRSA is suspected or if true penicillin/ beta-lactam allergy
- IV Vancomycin**
- If rapidly progressive, Add IV Clindamycin 600mg 6 hourly
- Duration 7-10 days (IV/oral)
Suspected Necrotising Fasciitis
- Consider SSTI with disproportionate pain or acute organ dysfunction/ hypoperfusion, including hypotension.
- Seek urgent surgical/orthopaedic review.
- Urgent DEBRIDEMENT/ EXPLORATION may be required
- IV Flucloxacillin 2g 6 hrly + IV Benzylpenicillin 2.4g 6 hrly + IV Metronidazole 500mg 8 hrly + IV Clindamycin 1.2g 6 hrly + IV Gentamicin**∆ (max 4 days)
- If MRSA is suspected or if true penicillin/beta-lactam allergy
- REPLACE Flucloxacillin + Benzylpenicillin with IV Vancomycin**
- Rationalise therapy within 48-72 hours
- Based on: response, microbiology results, infection specialist review
- Duration 10 days (IV/oral) or as per infection specialist
Infected human/animal bite
Non-severe bite
- Oral Co-amoxiclav 625mg 8 hrly or if true penicillin/beta-lactam allergy Oral ▲Doxycycline 100mg 12 hrly + Oral Metronidazole 400mg 8 hrly
- Duration 5 days (treatment) 3 days (prophylaxis)
Severe bite
- Consider surgical review.
- IV Co-amoxiclav 1.2g 8 hrly or if true penicillin/beta-lactam allergy
- IV Vancomycin** + Oral Metronidazole 400mg 8 hourly + Oral ▲■Ciprofloxacin 500mg 12 hourly
- Duration 7 Days (IV/oral)
Gastroenteritis
- Confirm travel history/ other risk factors
- Antibiotics are not usually required and may be deleterious in E.coli O157
- Consider viral causes, including COVID-19
difficile infection (CDI)
- See NHS GGC CDI guidance
- Treat before lab confirmation if suspected. Discontinue if toxin negative
No severity markers
- Oral Metronidazole 400mg 8 hrly
- (Do not use suspension)
Any severity marker or first recurrence of CDI
- Oral Vancomycin 125mg 6 hourly
- Duration 10 days
- If enteral feeding tube use Vancomycin (see complete NHS GGC CDI guidance)
Intra-abdominal sepsis
- IV Amoxicillin 1g 8 hrly + IV/Oral Metronidazole 500/400mg 8 hrly + IV Gentamicin**∆ (max 4 days) )
- If eGFR < 20 mL/min/1.73 m2 IV Piperacillin/Tazobactam 4.5g 12 hourly (Monotherapy)
- If true penicillin/beta-lactam allergy IV Vancomycin ** + IV/Oral Metronidazole 500/400mg 8 hourly + IV Gentamicin**Δ (max 4 days)
- If eGFR < 20mL/min/1.73 m2 ▲■ IV/Oral Ciprofloxacin + IV/Oral Metronidazole 500/400mg 8 hrly
- Total Duration 5 days (IV/oral)
- Assuming source control
Biliary tract infection
- As above, except metronidazole is not routinely required unless severe
Pancreatitis
- Does not require antibiotic therapy unless complicated by cholangitis.
Spontaneous bacterial peritonitis
- Ascites PLUS peritoneal white cell count > 500/mm3 or > 250 neutrophils/mm3
- If not receiving co-trimoxazole prophylaxis: IV/Oral Co-trimoxazole 960mg 12 hourly
- If receiving co-trimoxazole prophylaxis: IV Co-amoxiclav 1.2g 8 hrly or if true penicillin/beta-lactam allergy
- Oral /IV▲■Ciprofloxacin 500/400mg 12 hourly + IV Vancomycin**
- Duration 7 days (IV/oral)
Decompensated Chronic liver Disease with Sepsis Unknown Source
- IV Piperacillin/Tazobactam 4.5g 8 hourly or, if true, penicillin/beta-lactam allergy
- Oral /IV▲■Ciprofloxacin 500/400mg 12 hourly + IV Vancomycin**
- Duration 7 days (IV/oral)

UTI in Pregnancy
- See NHS GGC Obstetric guidance
Lower UTI/cystitis
- Don’t treat asymptomatic bacteriuria.
- Obtain urine culture before antibiotic.
- In women often self-limiting, consider delayed prescribing.
- Antibiotics if significant symptoms Oral Nitrofurantoin 50mg 6 hourly or Oral Trimethoprim 200mg 12 hourly
- Duration: Females 3 days, Males 7 days
- If eGFR < 30 mL/min/1.73 m2
- Nitrofurantoin contraindicated
- Trimethoprim use with caution may increase K+ and decrease renal function. Monitor
Upper UTI
- Obtain urine for culture before antibiotic. Exclude pneumonia if loin/back pain
Non-severe/without sepsis
- Oral▲■Ciprofloxacin 500mg 12 hourly or Oral Trimethoprim 200mg 12 hourly if sensitive organism.
- Duration 7 days
- Trimethoprim see above re lower eGFR
UROSEPSIS/ Pyelonephritis with fever
- IV Gentamicin**∆ (max 4 days) If eGFR < 20 mL/min/1.73 m2 Oral ▲■Ciprofloxacin
- Duration 7 days
Catheter-related UTI
- Remove/ replace catheter and send urine for culture. Don’t treat asymptomatic bacteriuria
Symptomatic bacteriuria without sepsis
- Give a single dose of IV Gentamicin**∆ immediately before catheter removal, or if the IV route is unavailable, give a single dose of oral ▲■Ciprofloxacin 500mg 30 minutes before catheter change. If eGFR 10-30 mL/min/1.73 m2 ▲■Ciprofloxacin 500mg single dose
Symptomatic bacteriuria with sepsis
- As above and treat as per pyelonephritis/ culture results.
- Duration 7 days (IV/oral)
Suspected prostatitis
- Consider in all men with lower UTI symptoms
- Refer to Urology
- Oral ▲■Ciprofloxacin 500mg 12 hourly or Oral Trimethoprim 200mg 12 hourly if sensitive organism.
- Duration 14 days

Septic arthritis/ Osteomyelitis Prosthetic joint infection
- Obtain blood cultures before antibiotic therapy. If not acutely unwell/septic, obtain synovial fluid/deep tissue samples before antibiotic treatment.
Native joint
- IV Flucloxacillin 2g 6 hrly If MRSA suspected or if true penicillin/beta-lactam allergy
- IV Vancomycin**
- If considered high risk for Gram-negative infection, e.g. immunocompromised, recurrent UTI or sickle cell disease
- ADD IV Gentamicin**∆ (max 4 days)
- Duration and IVOST: discuss with microbiology at 72 hours. Usually, 4 – 6 weeks (IV/oral) if the diagnosis is confirmed.
Prosthetic joint
- IV Vancomycin** + IV Gentamicin**∆ (max 4 days)
- Duration and IVOST: discuss with a microbiologist at 72 hours
Diabetic foot infection/ osteomyelitis
- Assess ulcer size, probes to the bone, neuropathy, peripheral vascular disease, and MRSA risk. For outpatient therapy, consult diabetic clinic guidelines IV Flucloxacillin 2g 6 hrly + IV/Oral Metronidazole 500/400mg 8 hourly. If SEPSIS or SIRS ≥2, Add IV Gentamicin**∆ (max four days)
- If MRSA is suspected or if true penicillin/beta-lactam allergy
- IV Vancomycin** + IV/Oral Metronidazole 500/400mg 8 hourly
- If SEPSIS or SIRS ≥2, Add IV Gentamicin**∆ (max four days) (Metronidazole oral bioavailability 80- 100%)
- If eGFR < 20 mL/min/1.73 m2
- REPLACE Gentamicin with Oral/IV ▲■Ciprofloxacin
- Duration/IVOST Discuss with Micro/ID
Vascular graft infection
- IV Flucloxacillin 2g 6hrly + IV Gentamicin**∆ (max four days)
- If MRSA is suspected or if true penicillin/beta-lactam allergy
- IV Vancomycin** + IV Gentamicin**∆ (max 4 days)
- Discuss duration/IVOST further management with an Infection specialist

Urgent Blood Cultures, then IV Antimicrobial Therapy within ONE hour.
- LP safe without CT scan UNLESS: seizures, GCS ≤ 12, CNS signs, papilloedema or immunosuppression. If CT: Blood cultures and antibiotics BEFORE CT scan.
- Use Meningitis/ Encephalitis order set on Trakcare, Blood and CSF Glucose. LP contraindicated if Brain shift, rapid GCS reduction, Resp/ cardiac compromise, severe sepsis, rapidly evolving rash, infection at LP site, coagulopathy, thrombocytopenia, anticoagulant drugs
Antibiotic Guidelines and Possible bacterial meningitis
- IV Ceftriaxone 2g 12 hrly
- or if true penicillin/beta-lactam allergy
- IV Chloramphenicol 25mg/kg (max 2g) 6 hrly
- If age ≥ 60 years, immunosuppressed, pregnant, alcohol excess, liver disease or if listeria meningitis suspected: ADD IV Amoxicillin 2g 4 hrly to Ceftriaxone
- or if true penicillin/beta-lactam allergy
- ADD IV Co-trimoxazole 30mg/kg 6 hrly to Chloramphenicol
- IF BACTERIAL MENINGITIS STRONGLY SUSPECTED ADD IV Dexamethasone 10mg 6 hourly (for four days) and referred to ID
- Duration of antibiotics: Discuss with Micro/ID
Possible viral meningitis
- Usually diagnosed after empirical management and exclusion of bacterial meningitis. Viral meningitis does NOT require antiviral prescription unless immunocompromised. Discuss with ID.
- Confusion or reduced consciousness = Encephalitis, NOT meningitis
Possible viral encephalitis
- Consider if confusion or reduced level of consciousness in suspected CNS infection. Ensure CSF viral PCR is requested. It may not be possible to differentiate it from bacterial meningoencephalitis. IV Aciclovir 10mg/kg 8 hrly
- See BNF for dosing in renal impairment.
- Discuss further management with ID/ virology. It may require repeat LP or neuro-imaging to establish the diagnosis.
- Duration: Discuss with ID

Urgent Blood Cultures, then IV Antimicrobial Therapy within ONE hour.
Community or Healthcare-associated sepsis was source unknown
- Review all anatomical systems, perform CXR and consider other imaging/ laboratory investigations
- Consider and test for COVID-19
- Review diagnosis DAILY
- Add cover for S.aureus infection if; healthcare-associated, recent hospitalisation, post-op wound/ line related, PWID
- Add cover for MRSA infection if; a recent MRSA carrier or previous infection
- Add cover for Streptococcal infection if; pharyngitis/erythroderma/hypotension
Source unknown
- IV Amoxicillin 1g 8 hrly + IV Gentamicin**∆ (max four days)
- If S.aureus suspected
- ADD IV Flucloxacillin 2g 6 hrly
- If MRSA is suspected or if true penicillin/ beta-lactam allergy
- IV Vancomycin** + IV Gentamicin**∆ (max 4 days)
- If severe Streptococcal infection suspected
- ADD IV Clindamycin 600mg 6 hourly
- If eGFR < 20 mL/min/1.73 m2 REPLACE
- Gentamicin with Oral/IV ▲■Ciprofloxacin
- Duration: Review with response/ micro results at 72 hours
Possible Infective Endocarditis
- Always seek senior specialist advice and refer to cardiology.
- Native heart valve
- IV Amoxicillin 2g 4 hrly + IV Flucloxacillin 2g 6 hrly if < 85kg (4 hrly if ≥ 85kg) + IV Gentamicin ∆ ( # synergistic dosing)
- If MRSA/ resistant organisms are suspected or if true penicillin/beta-lactam allergy
- IV Vancomycin** + IV Gentamicin ∆ (# synergistic dosing)
Prosthetic heart valve
- IV Vancomycin** + IV Gentamicin ∆ (# synergistic dosing)
- Discuss with Infection specialist within 72 hours
- # See Synergistic Gentamicin for Endocarditis in Adults guideline on StaffNet for dosing

Urgent Blood Cultures then IV Antimicrobial Therapy within ONE hour
Immunocompromised Patient
- Chemotherapy < 3 weeks, high dose steroids (e.g. prednisolone > 15mg/day for > 2 weeks), other immunosuppressants (e.g. anti-TNF, cyclophosphamide), Stem cell/solid organ transplant or primary immunodeficiency
Neutropenic Sepsis
- Neutrophils ≤ 0.5 x 109 / L + fever (temperature > 38°C or 37.5°C on 2 occasions 30 min apart) / hypothermia < 36°C OR chills, shivers, sweats or other symptoms suggestive of infection.
- All patients who have received recent chemotherapy and exhibit any of the symptoms above are presumed neutropenic and septic.
Immunocompromised with fever BUT normal neutrophils AND source of infection identified
- Manage as per infection management guidelines based on the anatomical source.
Neutropenic sepsis or Immunocompromised with fever and source of infection unknown;
- (See guideline Initial Management of Neutropenic Sepsis or Sepsis of Unknown Source in Immunocompromised Adults)
NEWS ≤ 6 Standard Risk
- IV Piperacillin/Tazobactam 4.5g 6 hourly
- If MRSA colonised/ line infection or sign of skin and soft tissue infection
- ADD IV Vancomycin** Or, if true, penicillin/ beta-lactam allergy
- IV Gentamicin**∆ (max 4 days) + IV Vancomycin**
NEWS ≥ 7 High Risk
- IV Piperacillin/Tazobactam 4.5g 6 hourly + IV Gentamicin**∆ (max 4 days)
- If MRSA colonised/ line infection or sign of skin and soft tissue infection
- ADD IV Vancomycin**
- Or if true penicillin/ beta-lactam allergy IV Gentamicin**∆ (max 4 days) + IV Vancomycin** + IV ▲■Ciprofloxacin 400mg 8 hourly
Patients with Stem Cell Transplants or receiving chemotherapy for Acute Leukaemia
- NEWS ≤ 6 See High-Risk treatment above. NEWS ≥ 7 Critical Risk See Neutropenic Sepsis guidelines
Important Antibiotic Drug Interactions & Safety Information!!
- ▲Doxycycline/ Quinolone: reduced absorption with iron, calcium, magnesium & some nutritional supplements. See BNF (Appendix 1) or see the pharmacy for advice.
- ■ Clarithromycin/ Quinolone: risk of severe drug interactions. See BNF (Appendix 1) or see the pharmacy for advice. May also prolong the QTc interval and avoid (where possible) other QTc risk factors.
- ▲■ Quinolones:g., Ciprofloxacin, levofloxacin stop treatment at first signs of a serious adverse reaction (e.g., tendonitis), prescribe with caution for people over 60 years and avoid co-administration with a corticosteroid. See BNF for dosing advice in reduced renal function.
** Gentamicin/ ** Vancomycin
- Gentamicin/ Vancomycin adult dosing calculators are available via the ‘Clinical Info’ icon on the staff intranet / CCC App. Use Prescribing, Administration, and Monitoring charts
- Vancomycin If creatinine is available, give Vancomycin loading dose as per actual body weight
- Gentamicin Avoid Gentamicin in decompensated liver disease or myasthenia gravis
| If creatinine is not available, give gentamicin as follows: | |||
| Actual Body Weight | Gentamicin Dose | Actual Body Weight | Gentamicin Dose |
| < 40 kg | 5 mg/kg | 60 – 69 kg | 320 mg |
| 40 – 49 kg | 240 mg | 70 – 79 kg | 360 mg |
| 50 – 59 kg | 280 mg | >, = 80 kg | 400 mg |
| NB if CKD5 give 2.5 mg/kg (max 180 mg) | |||
FURTHER ADVICE:
Duty Microbiologist, Clinical/ Antimicrobial Pharmacist, Infectious Disease (ID) Unit at QEUH, local Respiratory Unit (for RTI) or from the Adult Therapeutic Handbook. The Duty Microbiologist may give Infection Control advice.
Read More:
- Antimicrobial Stewardship School
- Sepsis Training Program
- Download Pocket Guide for Antibiotic Pharmacotherapy Book
- Microbiology Course | ABC Bacteria
- Infectious Disease E-News | FREE Subscription
- ABC antimicrobials | Know all about the Antimicrobials
- Road Map to Antimicrobial Stewardship Training Program
- Register Now in FADIC Clinical Research School
- FADIC Drug Information Fellowship
- Buy FADIC Toolkit for Writing Research to Write a Great Research Paper
- Read 10 Skills You Must Learn to Do Research via Google Scholar in Arabic
- Check Now FADIC Book store and Buy books in different specialities.
- FADIC Podcast focuses on varieties of pharmacist perspectives in different specialities.
- Download Now The Antibiotic Cards Book

 Log in
Log in Sign up
Sign up