CDI- Clostridium Difficile Infection
- CDI rates in the world have increased in the last decade, along with associated morbidity and mortality.
- It is an asymptomatic infection due to the spore-forming bacterium, Clostridium difficile(1).
- Clostridium Difficile, also known as C. difficile or C. diff, is a bacterium that can infect the bowel and cause diarrhoea.
- The infection most commonly affects people who have recently been treated with antibiotics but can spread quickly to others.
- C. difficile infections are unpleasant and can sometimes cause serious bowel problems, but they can usually be treated with another course of antibiotics (2)
Classification
- Clostridium difficile is more commonly referred to as a shortened version of C. diff. Clostridium is Greek for “Kloster” meaning spindle.
- Spindle refers to the rod shape of the bacterium. Also, C. difficile has been quite challenging to grow in a laboratory setting.
- Hence where it received the other half of its scientific name–“difficult” in Latin means “difficult”.
|
Domain: |
Bacteria |  |
| Kingdom: | Eubacteria | |
| Phylum: | Firmicutes | |
| Class: | Clostridia | |
| Order: | Clostridiales | |
| Family: | Clostridiaceae | |
| Genus: | Clostridium | |
| Species: | Clostridium difficile(3) |
General Characteristics of CDI
- CDI is found in nature in water, air, human and animal faeces, on most surfaces (especially in hospitals) and most prevalently in the soil.
- difficile shows optimum growth when at human body temperature (37˚C). C. difficile was first isolated by Hall and O’Toole from the meconium and faeces of newborn infants. (4)
- Its vegetative cells are rod-shaped, pleomorphic, and occur in pairs or short chains.
- Under the microscope, they appear as long, irregular (often drumstick- or spindle-shaped) cells with a bulge at their terminal ends (forms subterminal spores).
- Under Gram staining, C. difficile cells are Gram-positive and show optimum growth on blood agar at human body temperatures.
- When stressed, the bacteria produce spores that are able to tolerate extreme conditions that the active bacteria cannot take.
- difficile are anaerobic—live in the absence of oxygen. In the presence of oxygen. the vegetative form of C. difficile can survive up to 24 hours on an inanimate surface.
- whereas, C. difficile spores can survive up to 2 years on inanimate surfaces exposed to oxygen.
- It is catalase and superoxide dismutase negative,
- It produces two types of toxins: enterotoxin A and cytotoxin B, which disrupt cytoskeleton signal transductions in the host.
Highly recommend online Marketing tool from SEMRUSH
What are the Species of CDI?
- The Species of Clostridium are divided based on their sequences of genes coding for 16S rRNA.
- Species are also separated by the production of toxic and antigenic proteins.
- Their type of anaerobic metabolism, the percentage of G +C, and also on the basis of nucleic acid homologies. (3)
Genome
- It is essential to have C. difficile genome sequenced because it provides a better tool for preventing and controlling the infection.
- The genome also reveals clues as to how the pathogen thrives in the GI T and why some strains are so much more virulent than others.
- Genome of C. difficile can also explain their antimicrobial resistance and allow for quicker detection and better treatment options.
- In addition, it allows scientists to correlate different toxins and genes and their disease-causing ability. (6)
- Thus, strain 630 (epidemic type X) has a single circular chromosome with 4,290,252 bp (G+C content = 29.06%) and a circular plasmid with 7,881 bp (G+C content = 27.9%).
- The whole genome has been sequenced and found that 11% of the genome consists of mobile genetic elements such as conjugative transposons.
- Transposons are movable DNA fragments that can move from one location to another within the genome.
- These elements provide C. difficile with the genes responsible for its antimicrobial resistance, virulence, host interaction and the production of surface structures.
- For example, the idea gene of C. difficile produces a multidrug efflux pump.
- Which was shown to be homologous to known efflux transporters in the multidrug and toxic compound extrusion (MATE) family.
- The protein facilitates energy-dependent and sodium-coupled efflux of drugs from cells.
- In addition, the cme gene in C. difficile has been shown to provide multidrug resistance in other bacteria. (7,8)

Ecology
- C. difficile inhabits the microflora of the intestines of humans. Around 3% of healthy adults and up to 70% of babies have a number of C. difficile bacteria living in their gut.
- However, the number of C. difficile bacteria is kept very low and controlled by the millions of harmless bacteria in the intestines that aid digestion.
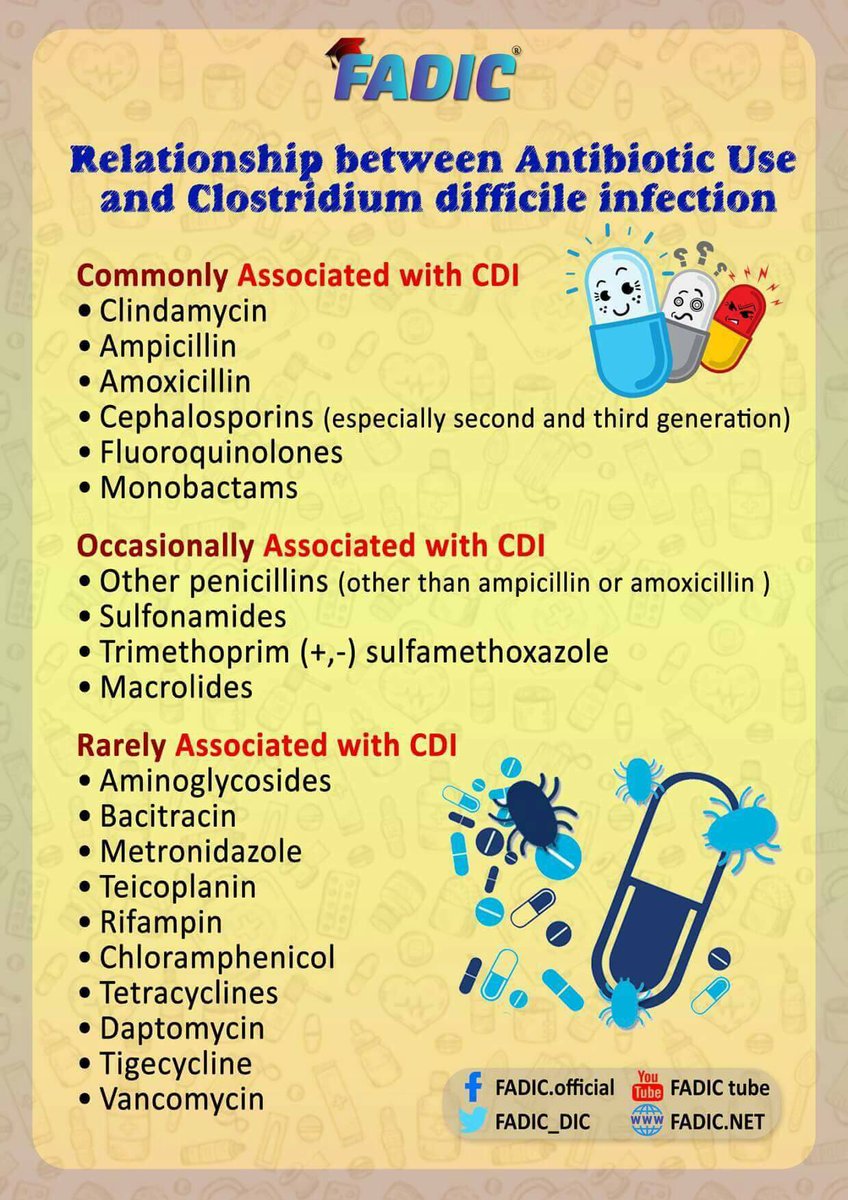
- C. difficile can grow in large populations in people that are treated with antibiotics, especially broad-spectrum antibiotics.
- This is because the antibiotics kill off the intestines’ normal flora, leaving C. difficile to freely grow and colonize the intestine Ideal condition for growth is around 37ºC (98.6 ºF).
- This explains why the human body plays the perfect host for C. difficile
- When under extreme conditions such as the low pH environment of the stomach.
- High heat or under attack by antibiotics, C. difficile can form spores that can survive for up to two years and withstand extreme conditions.
- The spores can then convert to the active form of C. difficile when conditions are favourable and allow the bacteria to grow. (9)
- In addition, when C. difficile undergoes stress (i.e. osmotic, acid and heat shock).
- Its ability to adhere increased (by increasing expression of surface proteins) allowing it to attach to human tissue cells more easily facilitating its colonization. (10)
Growth
- CDI reproduces by binary fission.
- The circular strand of DNA begins replicating.
- Then, the cell begins elongating as the new copies of DNA start to move to opposite ends of the cell.
- Once replication is finished, the cell continues to grow, and the plasma membrane begins to invaginate until a new cell wall establishes.
- The result is two identical daughter cells with an exact copy of the original cell’s DNA(11)

Movement
- difficult moves via peritrichous flagella.
- These flagella evenly spread around the surface of each cell and allow the bacteria to be highly motile.
- The bacteria can move in a tumbling motion and move in a forward direction.
Nutrition
- CDI is heterotrophic, meaning it cannot make its food and relies on organic substances for nutrition.
- Since C. difficile is anaerobic, it obtains its energy, ATP, by fermentation of carbon and nitrogen substrates and can utilize sugars.
- C. difficile requires six amino acids for fermentative metabolism and growth.
- The leucine, isoleucine, proline, tryptophan, valine, and glycine. glycine increases its growth significantly(12).
Adaptations
- difficile exists in two states—the vegetative (growth) form or the spore state.
- In the vegetative state, the bacterium is able to use nutrients to grow and divide. However, when conditions become unfavourable, C. difficile is able to enter a dormant state and form a highly resistant spore.
- Unfavorable conditions include deprivation of nutrients, exposure to a very acidic environment, or exposure to high temperatures.
- These spores are very resistant to heat, radiation, drying, chemicals, and even oxygen (for up to two years).
- The spore is dormant, and a thick spore coat protects its genetic material.
- When conditions become favourable again, the C. difficile spore is able to return to its vegetative state.
- The bacteria’s ability to form spores enables its survival through the human digestive system.
- In addition to out into the oxygenated environment until it returns to its human host and back into the vegetative state. (9)

Human Pathogen
- Clostridium Difficle enters a person’s body via ingestion of the spores via the faecal-oral route.
- After ingestion, spores travel unchanged through the stomach’s acidic environment and germinate into the vegetative form.
- Pathogenic C. difficile strains produce multiple toxins.
- The best characterized are enterotoxin (Clostridium difficile toxin A) and cytotoxin (Clostridium difficile toxin B).
- Both may produce diarrhoea and inflammation in infected patients (Clostridium difficile colitis), although their relative contributions have been debated. Toxins A and B are glucosyltransferases that target and inactivate the Rho family of GTPases.
- Toxin B (cytotoxin) induces actin depolymerization by a mechanism correlated with a decrease in the ADP-ribosylation of the low molecular mass GTP-binding Rho proteins.
- Another toxin, binary toxin, is also described, but its role in disease is not fully understood.
- Additional virulence factors include an adhesin factor which mediates the binding to human colonic cells and a hyaluronidase.
- also C. difficile acquired nosocomially (acquired secondary to a primary hospitalization).
- Because, in the hospital, patients are often on broad-spectrum antibiotic therapy to prevent any infection.
- Nevertheless, these antibiotics can cause pathogenic strains of C. difficile to grow out of control and cause C. difficile- associated disease or CDAD.(13,14)
Host Range
- The difficile infects pigs, calves, and humans, and inhabits a natural reservoir of soil, faeces of domestic animals and humans, sewage, the human intestinal tract, and retail meat. (15)
- A 2015 CDC study estimated that C. difficile afflicted almost half a million Americans and caused 29,000 deaths in 2011.
- The study estimated that 40 per cent of cases began in nursing homes or community health care settings, while 24 per cent occurred in hospitals. (1)
Signs And Symptoms
- Clostridium difficile infection (CDI) symptoms can range from mild diarrhoea to severe cases including pseudomembranous colitis and toxic megacolon and death. (1)
Diagnosis
- Prior to the advent of tests to detect C. difficile toxins, the diagnosis was most often made by colonoscopy or sigmoidoscopy.
- The appearance of “pseudomembranes” on the mucosa of the colon or rectum is highly suggestive, but not diagnostic of the condition. ( 16)
Clinically, CDI is diagnosed using tests such as:
- immunoassays (including enzyme immunoassays, enzyme-linked immunosorbent assays, and immunochromatography assay)
- tests for C. difficile toxins,
- amplification of C. difficile DNA, through means such as PCR and loop-mediated isothermal amplification (LAMP) (15)
Treatment
- Carrying C. difficile without symptoms is common.
- Treatment in those without symptoms is controversial.
- In general, mild cases do not require specific treatment.
- Oral rehydration therapy is useful in treating dehydration associated with diarrhoea (5)
- Several different antibiotics are used for C. difficile, with the available agents being more or less equally effective.
- Metronidazole typically is the initial drug of choice for mild to moderate disease, it is taken three times a day for ten days.
- Vancomycin by mouth is preferred for severe diseases. Additionally, vancomycin is used to treat mild-to-moderate disease if diarrhoea persists after a course of metronidazole.
- Since metronidazole has the potential to cause congenital disabilities.
- Pregnant women with Clostridium difficile infection treated with vancomycin regardless of disease severity.
- Typical vancomycin dosage is taken four times daily for ten days.
- Given rectally if the person develops an ileus and cannot take medications by mouth. (17)
- Fidaxomicin was found to be as effective as vancomycin in those with mild to moderate disease and may be better in those with severe disease.
- They are tolerated as well as vancomycin and may have a lower risk of recurrence.
- Used in those who have recurrent infections and have not responded to other antibiotics.
- Medications used to slow or stop diarrhoea, such as loperamide, may worsen C. difficile disease, so not recommended.
- Cholestyramine, an ion exchange resin, is effective in binding both toxin A and B, slowing bowel motility, and helping prevent dehydration.
- The Cholestyramine is recommended with vancomycin. A last-resort treatment in those who are immunosuppressed is intravenous immunoglobulin(18)
- The fidaxomicin: in 2011, the FDA approved a new agent, fidaxomicin, for the treatment of CDI.
Treatment for relapsed or recurrent CDI
- It is even more problematic. CDI recurs in 15 – 35 per cent of patients with one previous episode and 33 – 65 per cent of patients with more than two episodes.
- Currently, clinicians choose from several antibiotics, dosing protocols, and adjunctive treatments (such as antimicrobials, probiotics, toxin-binding agents, and immune-system enhancing agents).
- The goal of most adjunctive treatments is to reduce patient susceptibility to relapse or reinfection.
- Fecal microbiota transplantation (FMT): It is The transplantation of faecal bacteria, via enema, colonoscopy, or another method, from a healthy individual to a recipient ( CDI patient) to restore a healthy gut microbiota. in particular, has a significant clinical interest. (1)
Prevention
- Not all people who acquire C. difficile develop CDI; thus prevention measures can target reducing both the spread of the bacteria or spores and patient susceptibility to infection.
- One study statistically modelled CDI within the hospital setting and suggested that reducing patient susceptibility to infection is more effective in reducing CDI cases than lowering transmission rates.
- Recent prevention efforts have included antimicrobial stewardship and using environmental and infection control strategies.
- As well as seeking to improve the patient’s immune defences through healthy digestive function and gut flora and improved nutrition
# The developing CDI depends on a number of factors that allow colonization and toxin production, including
- failure of the immune defences,
- use of antibiotics, particularly broad-spectrum or multiple antibiotics, and changes to the intestinal microbiota.
- older age,
- comorbidities
- use of gastric acid suppressant medications.
# Preventing transmission of C. difficile within institutional
- hygiene protocols. Unfortunately, protocols for some targeted hospital-associated infections may not be effective against C. difficile. For example, the alcohol hand rubs routine is unsuitable for eliminating difficulties because it produces spores that can withstand hostile environments and resist alcohol hand rubs and other routine antiseptics. (1)
Read More:
- Antimicrobial Stewardship School
- Sepsis Training Program
- Download Pocket Guide for Antibiotic Pharmacotherapy Book
- Microbiology Course | ABC Bacteria
- Infectious Disease E-News | FREE Subscription
- ABC antimicrobials | Know all about the Antimicrobials
- Road Map to Antimicrobial Stewardship Training Program
- Register Now in FADIC Clinical Research School
- FADIC Drug Information Fellowship
- Buy FADIC Toolkit for Writing Research to Write a Great Research Paper
- Read 10 Skills You Must Learn to Make a Research via Google Scholar in Arabic
- The FADIC Online Continuous Medical Improvement Programs & Mini-Courses.
- Check Now FADIC Book store and Buy books in different specialities.
- Watch Now FADIC TV to Keep Yourself Updated.
- FADIC Podcast focusing on varieties of pharmacist perspectives in different specialities.
- Subscribe Now to FADIC 2020 Daily News (FNN) and Keep Updated.
- Check Now about Coronavirus Resource Information Center.
 Log in
Log in Sign up
Sign up
