Chronic Conditions: Definition, Management, and Pharmacist Counseling
Chronic Conditions: Definition, Management, and Pharmacist Counseling

Chronic Conditions
One of the most important elements of effective communication between people is sharing the same language.
This concept will be very important in the critical conversation, such as a conversation between a patient and his/ her doctors.
So doctors and patients need to know and understand the meaning of each word they use.
Moreover, Chronic Conditions are the most common term used in our daily conversation not only between patients and their doctors but also between each other.
However, chronic disease as a term is very confusing about its meaning at first and the time required for a disease to be present to refer as chronic disease.
Also there is a questions about their numbers and the base according to which doctors can classify a certain disease as a chronic disease.
On the other hand, we begin to discuss the chronic diseases, we need to know the meaning of disease at first.
Highly recommend online Marketing tool from SEMRUSH
What is “Disease”
A disease is a dependent continuant constituted of one or more causal chains of clinical disorders (abnormal states) that appear in a human body and is initiated by at least one disorder.
The diseases may be caused by internal factors as the internal dysfunctions or by external factors such as pathogens.
There are some evidences assume that diseases not isolated from each other although their clinical and pathological features are diversiform.
Understanding how diseases are related to each other can provide novel insights into etiology and pathogenesis.
Moreover, diseases have many classifications according to different bases.
One of the first attempts to establish a scientific classification was done by undertaken by Carolus Linnaeus.
He classified diseases into such categories as:
- exanthematic (feverish with skin eruptions),
- phlogistic (feverish with heavy pulse and topical pain)
- dolorous (painful).
The effort was largely a failure because of the lack of an adequate understanding of the biological basis of disease.
One of the most common classifications of the disease is according to their causes, they can be classified into:
- infectious diseases,
- deficiency diseases,
- hereditary diseases (including both genetic diseases and non-genetic hereditary diseases),
- Physiological diseases.
Diseases can also be classified in other ways according to transmission into:
- Communicable diseases ( transfer from person to another)
- Non-communicable diseases (NCD, NOT transfer from person to another) .
Another important classification is due to the time that diseases present in:
- chronic diseases
- acute diseases
Difference between Acute Diseases Vs. Chronic Diseases
- Firstly, Acute conditions are severe and sudden in onset.
- Secondly, This could describe anything from a broken bone to an asthma attack.
- Finally, A chronic condition, by contrast, is a long-developing syndrome, such as osteoporosis or asthma.
In addition to the osteoporosis, a chronic condition, may cause a broken bone, an acute condition.
Moreover, an acute asthma attack occurs in the midst of the chronic disease of asthma. Acute conditions, such as a first asthma attack, may lead to a chronic syndrome if untreated.

Different definitions of the chronic disease within the public internet sources:
If we begin with the popular Internet sources, MedicineNet describes a chronic disease as
“One lasting 3 months or more, by the definition of the U.S. National Center for Health Statistics.”
Chronic diseases generally cannot be prevented by vaccines or cured by medication, nor do they just disappear.
According to Wikipedia, a chronic condition is,
A human health condition or disease that is persistent or otherwise long-lasting in its effects or a disease that comes with time.
The term chronic is often applied when the course of the disease lasts for more than three months.
Common chronic diseases include arthritis, asthma, cancer, COPD, diabetes and viral diseases such as hepatitis C and HIV/AIDS
The different definition of chronic disease in the medical society
Unfortunately, each foundation has its own definition of chronic disease.
For example, the Centers for Disease Control (CDC) define chronic diseases:
“conditions that last 1 year or more and require ongoing medical attention or limit activities of daily living or both”
The list of Chronic Conditions according to CDC
- HPN
- Alzheimer’s Disease
- Heart Diseases
- Depression
- Arthritis
- Osteoporosis
- Diabetes
- COPD
- Cancer
- Stroke
Centers for Medicare and Medicaid Services
More extensive list of chronic conditions were mentioned by The Centers for Medicare and Medicaid Services.
That list includes:
- Alzheimer’s Disease and Related Dementia
- Heart Failure
- Arthritis (Osteoarthritis and Rheumatoid)
- Hepatitis (Chronic Viral B & C)
- Asthma
- HIV/AIDS
- Atrial Fibrillation
- Hyperlipidemia (High cholesterol)
- Autism Spectrum Disorders
- Hypertension (High blood pressure)
- Cancer (Breast, Colorectal, Lung, and Prostate)
- Ischemic Heart Disease
- Chronic Kidney Disease
- Osteoporosis
- Chronic Obstructive Pulmonary Disease
- Schizophrenia and Other Psychotic Disorders
- Depression
- Stroke
- Diabetes
NHS of Wales
In the UK, NHS of Wales defined the chronic diseases are those which in most cases cannot be cured, only controlled, and are often life-long and limiting in terms of quality of life.
They include:
- diabetes,
- chronic obstructive pulmonary disease,
- asthma,
- arthritis,
- epilepsy
- Coronary heart disease.
- stroke(
Australian Institute
On the other hand, the Australian Institute for Health and Welfare
Includes the following as common features of the chronic disease:
- Complex causality, with multiple factors leading to their onset
- A long development period, for which there may be no symptoms
- A prolonged course of illness, perhaps leading to other health complications
- Associated functional impairment or disability.
So, according to the Australian Institute, chronic diseases can range from mild conditions to life-threatening heart disease and cancers.
Examples of chronic diseases include:
- Cardiovascular conditions (such as coronary heart disease and stroke)
- Cancers (such as lung and colorectal cancer)
- Many mental disorders (such as depression)
- Diabetes
- Many respiratory diseases (including asthma and COPD)
- Musculoskeletal diseases (arthritis and osteoporosis)
- Chronic kidney disease
- Oral Diseases.
World Health Organization
Finally, the World Health Organization states that chronic diseases are not passed from person to person.
They are of long duration and generally slow progression. The four main types of chronic diseases are
- cardiovascular diseases (like heart attacks and stroke),
- cancers,
- chronic respiratory diseases (such as chronic obstructed pulmonary disease and asthma)
- diabetes
Chronic disease: on the spot
chronic diseases are also known as, Noncommunicable diseases (NCDs), tend to be of long duration disease.
In addition to, they are the result of a combination of genetic, physiological, environmental and behaviours factors.
Noncommunicable diseases (NCDs) kill 41 million people each year, equivalent to 71% of all deaths globally.
Each year, 15 million people die from NCD between the ages of 30 and 69 years; over 85% of these “premature” deaths occur in low- and middle-income countries.
Cardiovascular diseases account for most NCD deaths, or 17.9 million people annually, followed by cancers (9.0 million), respiratory diseases (3.9million), and diabetes (1.6 million).
According to the 2010 National Survey of Residential Care Facilities (NSRCF) in the US, the most 10 common chronic conditions among persons living in residential care facilities were
National Survey of Residential Care Facilities (NSRCF)
- High blood pressure (57% of the residents),
- Alzheimer’s disease or other dementias (42%),
- Heart disease (34%),
- Depression (28%),
- Arthritis (27%),
- Osteoporosis (21%),
- Diabetes (17%),
- COPD and allied conditions (15%),
- Cancer (11%),
- Stroke (11%)
What is the risk factor of such diseases?
People of all age groups, regions and countries are affected by NCDs.
These diseases are often associated with older age groups.
Even though evidence shows that 15 million of all deaths attributed to NCDs occur between the ages of 30 and 69 years.
In addition to the children, adults and the elderly are all at risk.
The risk of having chronic disease increases by unhealthy diets, physical inactivity.
It may show up in people as raised blood pressure, increased blood glucose (hyperglycemia), elevated blood lipids (hyperlipidemia) and obesity.
These are called metabolic risk factors that can lead to cardiovascular disease, the leading NCD in terms of premature deaths.
There are also other risk factors called modifiable behavioural risk factors.
Moreover, these factors include tobacco use, the harmful use of alcohol and the excessive use of salt.
Tobacco accounts for over 7.2 million deaths every year (including from the effects of exposure to second-hand smoke).
4.1 million annual deaths have been attributed to excess salt/sodium intake.
Can we prevent or control chronic diseases?
An important way to control NCDs is to focus on reducing the risk factors associated with these diseases.
Monitoring progress and trends of NCDs and their risk is important for guiding policy and priorities.
In addition to the Investing in better management of NCDs is critical.
Management of NCDs includes detecting, screening and treating these diseases, and providing access to palliative care for people in need.
High impact essential NCD interventions can be delivered through a primary health care approach to strengthening early detection and timely treatment.
Evidence shows such interventions are excellent economic investments because, if provided early to patients, they can reduce the need for more expensive treatment.
The management of chronic disease
Disease management approach is increasingly advocated as a means of improving the effectiveness and efficiency of healthcare for chronic diseases.
Chronic Disease Management can provide support from a range of medical and allied health services, including:
- physician consultation
- diabetes education
- nutrition advise from a qualified dietitian
- support, counselling and information about community resources from a social worker
- proper use of medications for better disease control, decreasing disease-related complications and improving overall health
- a personalized exercise program developed by a physiotherapist
- an occupational therapist, who can assist the patient maintain his/ her independence in daily activities.
Chronic Disease Management plans
There are two types of plans that can be prepared by a General Practitioner (GP) for Chronic Disease Management:
- GP Management Plan (GPMP
- Team Care Arrangements (TCAs).
GP Management Plan
A GP Management Plan (GPMP) can help people with chronic medical conditions by providing an organized approach to care.
A GPMP is a plan of action the patient have agreed with his / her GP. This plan:
- Identifies the general health condition of patient and care needs;
- Sets out the services to be provided by GP; and
- Lists the actions the patient can take to help manage his / her condition.
Team Care Arrangements
If the patient has a chronic medical condition and complex care needs requiring multidisciplinary care, the GP may also develop Team Care Arrangements (TCAs).
Moreover, these will help coordinate more effectively other health care providers.
TCAs require GP to collaborate with at least two other health or care providers who will give ongoing treatment or services
Pharmacists role in the Chronic Disease Management

Medication therapy management (MTM)
Medication therapy management (MTM) is one form of a medication benefit program offered by public and private health providers and insurers.
Although the term was first coined in 2003, MTM in its earlier forms has been used since the 1990s as a mechanism to improve health metrics for medically complex patients.
An MTM service includes:
- Comprehensive medication review to ensure that the patient’s medication-related needs have been met
- At the end of the visit, a care plan is developed and shared with the patient and the primary care provider to resolve and prevent any drug therapy problems
Pharmacists have been shown to positively impact chronic disease outcomes through medication therapy management (MTM), which involves:
- Multifaceted approach of reviewing medications,
- Identifying and remedying medication-related problems
- Providing disease state management and self-management education
- Addressing medication adherence issues
- Considering preventative health strategies to optimize medication-related health.
Chronic Conditions for Medication Therapy Management
- Alcohol Use Disorder
- Alzheimer’s Disease and Related Disorders or Senile Dementia
- Anaemia (Includes Sickle Cell Disease)
- Atrial Fibrillation
- Asthma
- Bipolar Disorder
- Cancer – All Inclusive
- Cataract
- Chronic Kidney Disease
- Chronic Obstructive Pulmonary Disease and Bronchiectasis
- Cystic Fibrosis
- Deep Venous Thrombosis (DVT) (while on anticoagulation)/Pulmonary Embolism ( PE) (chronic anticoagulation)
- Depression
- Diabetes Mellitus
- Glaucoma
- Heart Failure
- Haemophilia
- HIV
- Hyperlipidemia
- Hypertension
- Ischemic Heart Disease
- Lead Exposure
- Liver Disease, Cirrhosis and Other Liver Conditions (except Viral Hepatitis)
- Obesity
- Osteoporosis
- RA/OA (Rheumatoid Arthritis/Osteoarthritis)
- Schizophrenia, Schizotypal, Delusional, and Other NonMood Psychotic Disorders
- Stroke/Transient Ischemic Attack
- Substance Use Disorder
- Tobacco Use Disorder
- Viral Hepatitis
Example of MMT: Managing Chronic Kidney Disease with MTM
Care for the chronic kidney disease (CKD) patient poses unique challenges to prescribers and practitioners.
Patients with CKD present with comorbid conditions such as diabetes, hypertension, anaemia, osteodystrophy, and electrolyte disturbances.
This can result in problematic situations due to:
- multiple physicians often prescribe a CKD patient’s medications.
- gaps in communication between healthcare providers that cause medication-related problems (MRP)
- the unfamiliarity of disease-state management by the patient
- complex medication regimens have been found to impair adherence to medication therapy.
Patients with CKD may experience significant MRPs.
Moreover, patients with end-stage renal disease (ESRD) undergoing dialysis, have complex medication regimens and are at a higher risk for MRPs.
These MRPs result in significant morbidity, mortality, and excessive cost to the healthcare system.
CKD patients are generally managed by a primary care provider, nephrologist, social worker, dietitian, nurse, and pharmacist.
Although all healthcare providers share the same goal of preventing kidney disease progression, gaps occur in the care of these patients.
Cause of Non-adherence
There is a piece of growing evidence that supports the involvement of a nephrology-trained clinical pharmacist closing these gaps in this patient population.
Medication non-adherence, particularly in the elderly and those with chronic comorbidities, can lead to increased costs, worsening disease progression, adverse effects, and hospitalisations.
Patient adherence can be affected by many factors including patient beliefs, including prioritisation and concerns about side effects and efficacy of medications.
Other factors such as forgetfulness, low health literacy, cost, and lack of information also may affect patient adherence.
Physicians and other healthcare providers may potentially contribute to patient non-adherence by prescribing complex medication regimens, inadequately providing proper communication and counselling on the risks and benefits of these medications, and failing to consider the cost of therapy.
Pharmacists have the opportunity to play a key role in educating patients and addressing these communication gaps between patients, physicians, and the healthcare system in order to help reduce MRPs and improve medication adherence.
So that the role of the pharmacist can positively impact the overall care of the CKD patient through the provision of clinical services targeted toward safe and efficacious outcomes in terms of MTM
Clinical pharmacists
Increased involvement of clinical pharmacists in patient care may offer increased access to primary care services and improved health care for patients.
Furthermore, pharmacist involvement in patient care may help to reduce inappropriate medication use, specifically in the elderly.
Community pharmacists
Community pharmacists can improve disease management improving the effective use of medicines and by reducing the occurrence of adverse drug reactions (ADRs).
Pharmacists working in community pharmacy have an added advantage of detecting and reporting ADRs while dealing with on the counter prescriptions
Pharmacists at the CCDMC
Studies have shown that integrating pharmacists into ambulatory clinics can improve chronic disease management and optimal use of medications.
Pharmacists at the CCDMC play a vital role as medication therapy management experts.
The Complex Chronic Disease Management Clinic (CCDMC) is a multidisciplinary ambulatory clinic staffed by nurse clinicians, pharmacists, and internal medicine physicians.
It was established in 2008 to enhance access to specialized medical services for patients with a history of multiple hospital admissions.
Its purpose is to reduce exacerbations of chronic conditions, visits to the emergency department, and acute care admissions.
The CCDMC pharmacists are responsible for a wide variety of patient-centred activities including:
- medication reconciliation
- detecting drug interactions
- ordering laboratory tests to monitor drug therapy
- prescribing, adapting, and extending prescriptions
- providing patient education.
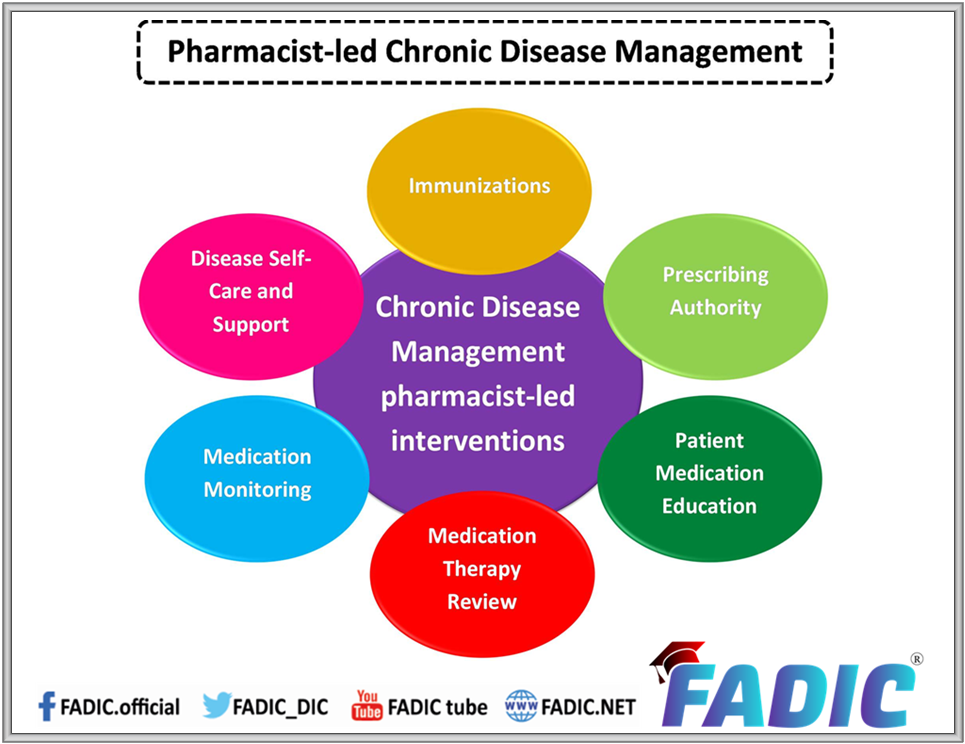
Pharmacist-led Chronic Conditions Disease Management
Chronic disease management is a multi-component intervention.
An intervention done by a pharmacist called pharmacist-led chronic disease management for community-dwelling adults with chronic diseases.
In addition to, it is a type of care that can be provided by pharmacists and aims to control symptoms and slow or stop disease progression.
The pharmacists’ intervention components are summarised in the following graph:
Comprehensive medication management (CMM)
According to the World Health Organization, adherence to therapy for chronic diseases in developed countries averages 50%.
Poor adherence to therapies results in poor health outcomes and increased health care costs.
So, Medication adherence is viewed as an essential component of effective chronic disease treatment.
In addition to the clinical pharmacists are certainly trained, qualified, and eligible to resolve non-adherence problems.
However, the more influential problems require the unique expertise of a clinical pharmacist to enable the patient to achieve therapeutic goals.
This is known as comprehensive medication management (CMM)
What is CMM?
CMM is defined according to The American College of Clinical Pharmacy (ACCP) as the standard of care that ensures each patient’s medications is appropriate for the patient’s medical condition.
CMM includes an individualized care plan that achieves the intended goals of therapy with appropriate follow-up to determine actual patient outcomes.
This all occurs because the patient understands, agrees with, and actively participates in the treatment regimen.
How is CMM delivered?
Clinical pharmacists work in collaboration with other providers to deliver CMM that optimises patient outcomes.
Care is coordinated among providers and across systems of care as patients transition in and out of various settings.
The clinical pharmacist’s process of care comprises the following components:

The value of CMM realised in multiple ways by multiple groups.
Most importantly, patients benefit from improved medication-related clinical outcomes.
Patients also benefit directly from the increased individualised attention to medications and their impact on their daily lives.
Physicians and other care team members benefit when clinical pharmacists apply their pharmacotherapeutic expertise to help manage complex drug therapies.
Moreover, the physicians can dedicate more time to the diagnostic and treatment selection process, enabling them to be more efficient.
Patient counselling in Chronic Conditions
Patient compliance defined as the adherence of a patient towards the prescriber’s instructions.
In addition to, it means an understanding of how the medicine used, as well as a positive behaviour in which the patient motivated to use the treatment properly.
Moreover, the effective patient counselling makes the patient understand his/her illness, necessary lifestyle modifications and pharmacotherapy and thus enhance patient compliance.
So, Patient counselling defined as providing medication information orally or in written form to the patients and providing proper directions of use, advice on side effects, storage, diet and lifestyle modifications.
It involves a one-to-one interaction between a pharmacist and a patient and/or a caregiver. It is interactive in nature.
The effective counselling should make the patient/party understand his/her disease, medications and lifestyle modification required.
The Pharmacists role in patient counselling in Chronic Conditions
Importantly, pharmaceutical care defined as ” the responsible provision of drug therapy for the purpose of achieving definite outcomes that improve the patients’ quality of life”.
One of the important aspects of pharmaceutical care is counseling patients concerning medications.
Moreover, it has the responsibility of pharmacists to counsel the patients before dispensing the medication.
The counselling pharmacist should possess adequate knowledge and should be an effective communicator.
In addition to several guidelines published regarding the points covered while counseling the patients.
The Omnibus Budget Reconciliation Act (OBRA) 1990, (OBRA 1990, 1990) guidelines specify that the pharmacist should discuss at least the following points while counseling the patients:
- Name and description of the medication, the dosage form, route of administration
- Duration of therapy,
- Special precautions for preparation
- Common side effects or adverse effects or
- Drug interactions
- Therapeutic contraindications that may encountered, including their avoidance, and the action required if they occur,
- Techniques of self-monitoring of drug therapy, proper storage, prescription refill information, action taken in case of a missed dose.
Techniques of counselling in Chronic Conditions
Several techniques adopted for effective counseling.
In addition to some of them include providing written information to the patient and the use of audiovisual materials.
The use of various aids include labelling, medication calendars, drug reminder chart and providing special medication containers and caps also adopted.
In addition to the United States Pharmacopoeia (USP) medication counseling behaviour guidelines divide medication counseling into the following four stages.
Stage I: Medication information transfer,
During which there is a monologue by the pharmacist providing basic, brief information about the safe and proper use of medicine.
Stage II: Medication information exchange.
During which the pharmacist answers questions and provides detailed information adapted to the patients’ situation.
Stage III: Medication education.
During which the pharmacist provides comprehensive information regarding the proper use of medicines in a collaborative, interactive learning experience.
Stage IV: Medication counseling.
During which the pharmacist and patient have a detailed discussion intending to give the patient guidance that assists with proper management of medical conditions and effective use of medication.
The role of functional medicine in Chronic Conditions
Any time you’re in a conversation with patients with chronic illness, the topic of bound to come up.
For patients who live with constant pain, fatigue, and felling unwell, it may seem to make sense to turn to alternative treatment as another solution.
This done especially when traditional medicine not meet the patient expectations.
Additionally, according to Foundation for sarcoidosis research functional medicine is defined as
“medical practice or treatments that focus on optimal functioning of the body and its organs, usually involving systems of holistic or alternative medicine.”
Often, functional medicine promises a patient-centric approach, looking to address the root of any problems the patient has.
So that, The Functional Medicine model is an individualised, patient-centered, science-based approach that empowers patients and practitioners to work together.
This is to address the underlying causes of disease and promote optimal wellness.
It requires a detailed understanding of each patient’s genetic, biochemical, and lifestyle factors
What is the benefit of using The Functional Medicine model?
Firstly, by addressing root cause of the illness, rather than symptoms, additionally practitioners become oriented to identifying the complexity of disease.
Functional Medicine treatment targets the specific manifestations of disease in each individual.
On the other hand, one condition has many different causes.
Moreover, one cause may result in many different conditions.
As a result a diagnosis can be the result of more than one cause.
For example, depression can caused by many different factors, including inflammation.
Likewise, a cause such as inflammation may lead to a number of different diagnoses, including depression.
Importantly, the precise manifestation of each cause depends on the individual’s genes, environment, and lifestyle.
Not only that, only treatments that address the right cause will have lasting benefit beyond symptom suppression.
Read More:
- Antimicrobial Stewardship School
- Sepsis Training Program
- Download Pocket Guide for Antibiotic Pharmacotherapy Book
- Microbiology Course | ABC Bacteria
- Infectious Disease E-News | FREE Subscription
- ABC antimicrobials | Know all about the Antimicrobials
- Road Map to Antimicrobial Stewardship Training Program
- Register Now in FADIC Clinical Research School
- FADIC Drug Information Fellowship
- Buy FADIC Toolkit for Writing Research to Write a Great Research Paper
- Read 10 Skills You Must Learn to Make a Research via Google Scholar in Arabic
- The FADIC Online Continuous Medical Improvement Programs & Mini-Courses.
- Check Now FADIC Book store and Buy books in different specialties.
- Watch Now FADIC TV to Keep your self Updated.
- FADIC Podcast focusing on varieties of pharmacist perspectives in different specialties.
- Subscribe Now in FADIC 2020 Daily News (FNN) and Keep Updated.
- Check Now about Coronavirus Resource Information Center.

 Log in
Log in Sign up
Sign up