Dexamethasone | Coronavirus Disease COVID-19
Dexamethasone Use in Coronavirus Disease COVID-19
Mira Milad, Rasha Abdelsalam Elshenawy
What is Dexamethasone?
- Dexamethasone, a synthetic glucocorticoid, has anti-inflammatory and immunosuppressive properties
Benefits of Dexamethasone | Coronavirus Disease COVID-19
- Use of corticosteroids may prevent an extended cytokine response
- May accelerate resolution of pulmonary and systemic inflammation in pneumonia
- May improve dysregulated immune response caused by sepsis (possible complication of infection with COVID-19)
- Increase BP when low
Cytokine Storm:
- Evidence suggests that cytokine storm, a hyper-inflammatory state resembling secondary hemophagocytic lympho histiocytosis (HLH).
- This is a contributing factor in COVID-19- associated mortality.
- Immunosuppression from corticosteroids proposed as a treatment option for such hyperinflammation.
Clinical trials of Dexamethasone | Coronavirus Disease COVID-19
- Systemic corticosteroid therapy studied in several randomised controlled studies.
- Trials are for the treatment of ARDS.
- The overall evidence is low to moderate in quality and most studies performed prior to widespread implementation of lung protection strategies
Observational studies:
- Evidence suggests that corticosteroid use in patients with SARS, MERS, and influenza was associated with no survival benefit and possible harm.
- Harms (e.g., delayed viral clearance, avascular necrosis, psychosis, diabetes).
Uncontrolled observational data from China:
- Suggest a possible treatment benefit of methylprednisolone in COVID-19 patients with acute respiratory distress syndrome (ARDS).
Pending results of randomised controlled clinical studies:
- Specifically evaluating corticosteroids for COVID-19, indirect evidence from studies in patients with community acquired pneumonia.
- Additionally, ARDS, and other viral infections used to inform treatment decisions for COVID-19 patients.
In a recent multi-center, unblinded, randomised controlled study (DEXA-ARDS):
- The effects of Dexamethasone | Coronavirus Disease COVID-19 in conjunction with conventional care were evaluated in hospitalised patients with moderate-to severe ARDS receiving lung-protective mechanical ventilation.
- Treatment with IV dexamethasone at a dosage of 20 mg once daily on days 1-5, followed by 10 mg once daily on days 6-10 resulted in reduced duration of mechanical ventilation and reduced overall mortality (i.e., 15% increase in 60-day survival) compared with conventional treatment alone.
- Based on results of this study, a randomised controlled open -label trial (NCT04325061; DEXA-COVID19) initiated to specifically evaluate the use of IV dexamethasone at the same dosage of 20 mg once daily on days 1-5.
- It followed by 10 mg once daily on days 6-10 in patients with ARDS due to COVID-19.
A large open-label, randomised controlled trial
(NCT04381936; RECOVERY)
- Conducted to evaluate the effect of potential treatments (including low-dose dexamethasone) on all-cause mortality in hospitalised patients with COVID-19.
- The study enrolled over 11,500 patients with suspected or confirmed COVID-19 from over 175 hospitals in the UK.
- In the Dexamethasone Use in Coronavirus treatment arm, 2104 patients randomised to receive dexamethasone.
- The dose is (6 mg once daily orally or IV for 10 days) plus standard care and 4321 patients randomised to receive standard care alone.
- Sponsor announced that preliminary data analysis indicated that dexamethasone reduced 28-day mortality by 17%.
- In addition to the greatest benefit observed among patients requiring mechanical ventilation.
- Dexamethasone reduced mortality by one-third in patients requiring mechanical ventilation by one-fifth in other patients receiving oxygen only.
- However, there was no evidence of benefit in patients who not require respiratory support.
- Note: Confirmation of these results is pending until completion of full data analysis and publication of the final report
The effect of corticosteroid treatment on patients with coronavirus infection:
A systematic review and meta-analysis
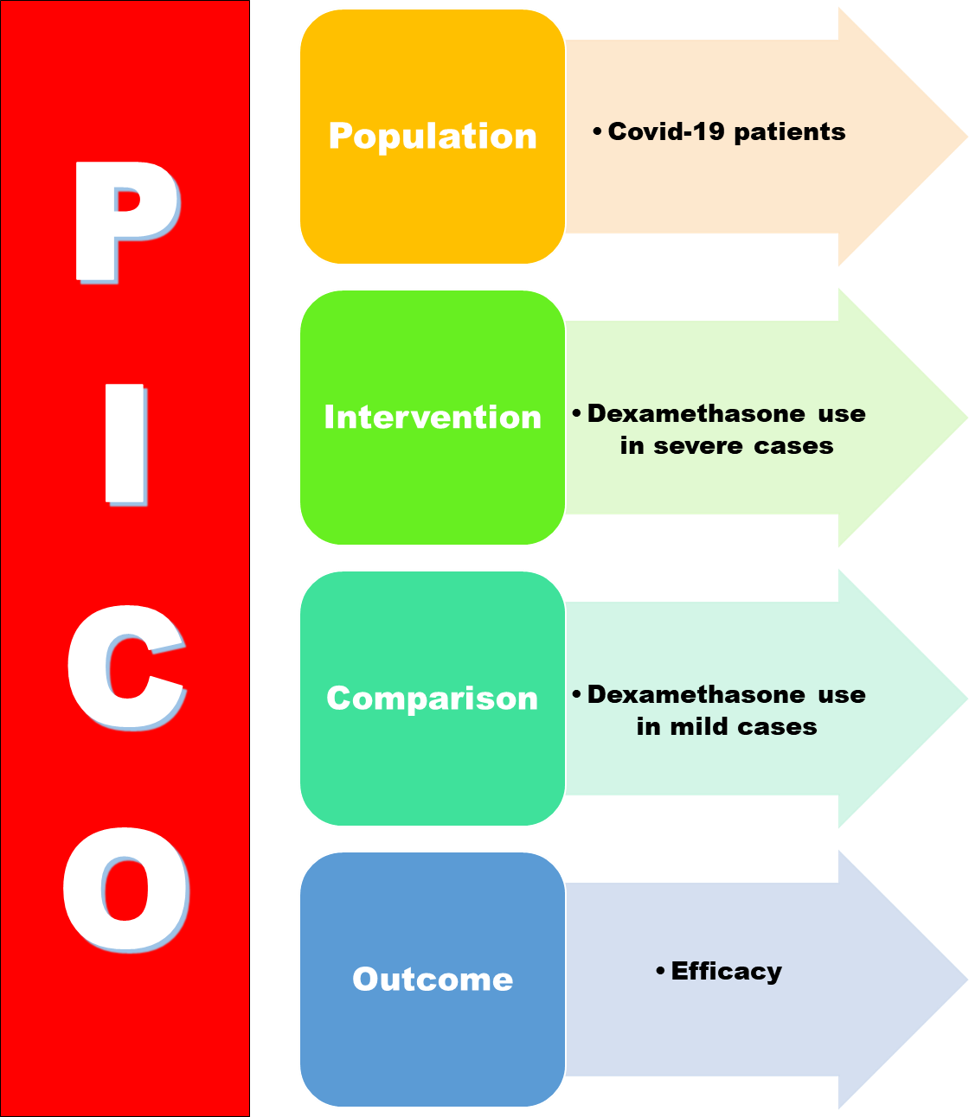
- Patients with severe conditions more likely to require corticosteroids.
- Corticosteroids could lead to higher mortality, longer LOS, a higher rate of bacterial infection and hypokalemia.
- Therefore, corticosteroid should used with caution in the treatment of COVID-19 patients corticosteroids are not recommended for patients with mild conditions
- Moderate corticosteroids can used in patients with severe conditions to suppress the immune response and reduce symptoms.
- Nevertheless, more multi-center clinical trials needed to further verify this conclusion.
Other clinical trials
- Have been initiated in various countries to evaluate use of IV corticosteroids (e.g., dexamethasone, hydrocortisone).
- Additionally, oral corticosteroids (e.g., prednisone), or inhaled corticosteroids (e.g., budesonide, ciclesonide) for treatment of COVID-19 pneumonia or ARDS.
- Randomised controlled studies evaluating use of corticosteroids (e.g., hydrocortisone, dexamethasone, methylprednisolone, prednisolone) in septic shock suggest a small, but uncertain mortality reduction
Dosage of Dexamethasone | Coronavirus Disease COVID-19
- In general, low to moderate dosages of corticosteroids recommended in intubated patients with ARDS.
- Regimens used in China were typically methylprednisolone 40-80 mg IV daily for a course of 3-6 days.
- Some experts suggest that equivalent dosages of dexamethasone (i.e., 7-15 mg daily, typically 10 mg daily) may have an advantage of producing less fluid retention, since dexamethasone has less mineralocorticoid activity.
- This dosage of dexamethasone consistent with those used in the DEXA-ARDS trial.
- However, lower dosages of dexamethasone (i.e., 6 mg once daily for 10 days) were used in the RECOVERY trial.
- Higher dosages suggested for cytokine storm
Comments:
- Data on the use of corticosteroids in COVID-19 are limited.
- The benefits and risks of corticosteroid therapy should carefully weighed before use in patients with COVID-19
- NIH, CDC, WHO, IDSA, and other experts have issued guidelines for the use of corticosteroids in patients with COVID19 based on the currently available information.
- Recommendations made according to the severity of illness, indications, and underlying medical conditions and should be considered on a case-by-case basis.
General Recommendation of Dexamethasone | Coronavirus Disease COVID-19:
- General recommendations: WHO, CDC, NIH, and IDSA generally recommend against the routine use of corticosteroids for the treatment of COVID-19 unless indicated for another reason (e.g., asthma or COPD exacerbation, refractory septic shock).
- NIH recommends against the routine use of systemic corticosteroids for the treatment of COVID-19 in hospitalised patients unless they are in the intensive care unit.
- NIH also recommends against the routine use of systemic corticosteroids for the treatment of mechanically ventilated COVID-19 patients without ARDS.
- However, the NIH panel states that there is insufficient evidence for or against the use of systemic corticosteroids in mechanically ventilated patients with COVID-19 and ARDS.
- IDSA suggests against using corticosteroids in hospitalised patients with COVID -19 pneumonia.
- Besides, in those with ARDS due to COVID-19, systemic corticosteroids may used in the context of a clinical trial.
- Critically ill patients: The Surviving Sepsis Campaign COVID-19 subcommittee (a joint initiative of the Society of Critical Care Medicine and the European Society of Intensive Care Medicine) recommends against the routine use of systemic corticosteroids in mechanically ventilated adults with COVID-19 and respiratory failure (without ARDS).
- However, these experts generally support a weak recommendation to use low-dose, short-duration systemic corticosteroids in the sickest patients with COVID-19 and ARDS.
Non-critical Patients:
- Non-critical patients: Corticosteroids generally should not used in the treatment of early or mild disease.
- Since the drugs can inhibit immune response, reduce pathogen clearance, and increase viral shedding.
- Clinicians considering corticosteroids for such patients with COVID-19 should balance the potential small reduction in mortality with potential effects of prolonged coronavirus shedding
- If corticosteroids are prescribed, monitor and treat adverse effects including hyperglycemia, hypernatremia, and hypokalemia.
Cytokine storm:
- There is no well-established or evidence-based treatment for cytokine storm in patients with COVID-19.
- However, some experts suggest that use of more potent immunosuppression with corticosteroids may be beneficial in such patients.
- These experts suggest higher dosages of corticosteroids (e.g., IV methylprednisolone 60-125 mg every 6 hours for up to 3 days) followed by tapering of the dose when inflammatory markers (e.g., C-reactive protein levels) begin to decrease.
- The decision to use corticosteroids in patients with early signs of cytokine storm should be balanced with the known adverse effects.
Septic shock:
- The effect of corticosteroids in COVID-19 patients with sepsis or septic shock may be different than the effects seen in those with ARDS.
- The Surviving Sepsis Campaign and NIH suggest the use of low-dose corticosteroid therapy.
- Examples of these doses are (e.g., hydrocortisone 200 mg daily as an IV infusion or intermittent doses).
- When used over no corticosteroid therapy in adults with COVID-19 and refractory shock.
Comorbidities:
Patients receiving corticosteroid therapy for chronic conditions:
- NIH states that oral corticosteroids used for the treatment of an underlying condition prior to
- COVID-19 infection (e.g., primary or secondary adrenal insufficiency, rheumatologic diseases) should not be discontinued.
- The guidelines also recommend that inhaled corticosteroids used daily for the management of asthma and COPD.
- It used to control airway inflammation should not discontinued in patients with COVID-19.
Rheumatology experts, including members of the American College of Rheumatology COVID-19 Clinical Guidance Task Force
- state that abrupt discontinuance of corticosteroid therapy in patients with rheumatologic diseases should avoided regardless of COVID19 exposure or infection status
Endocrinology experts
- They state that patients with primary or secondary adrenal insufficiency who are receiving prolonged corticosteroid therapy should follow usual steroid.
- If such individuals develop symptoms such as fever and a dry continuous cough.
- They should immediately double their daily oral corticosteroid dosage and continue with this regimen until the fever subsides.
- These guidelines also apply to patients who are receiving prolonged therapy (> 3 months) with corticosteroids for underlying inflammatory conditions, including asthma, allergy, and rheumatoid arthritis.
- In such patients whose condition worsens or in those experiencing vomiting or diarrhoea, treatment with parenteral corticosteroids may necessary.
Pregnancy considerations:
- For pregnant women with COVID-19, NIH guidelines state that the antenatal use of corticosteroids that cross the placenta.
- Examples (i.e., betamethasone, dexamethasone) generally reserved for when administration is required for fetal benefit.
- ACOG recommends against administration of antenatal corticosteroids for fetal benefit in the late preterm period.
- (i.e., 34 weeks and 0 days through 36 weeks and 6 days) in patients with suspected or confirmed COVID-19.
- Because the benefits of such therapy in late preterm less well established.
- Treatment should individualised, weighing the neonatal benefits of antenatal corticosteroid therapy with the risks of potential harm to the pregnant patient.
Conclusions:
- Dexamethasone “the only drug that’s so far shown to reduce mortality AND it reduces it significantly.
- This is the first treatment shown to reduce mortality in patients with COVID-19 requiring oxygen or ventilator support.
- If patients who have COVID-19 and are on ventilators or on oxygen given dexamethasone, it will save lives.
- For patients on ventilators, the treatment shown to reduce mortality by about a third.
- For patients requiring only oxygen, deaths were cut by about one fifth.
- Among patients with COVID-19 who not require respiratory support, there was no benefit from treatment with dexamethasone.
N.B. Methylprednisolone, a steroid similar to but less potent than dexamethasone.
Read More:
- The FADIC Online Continuous Medical Improvement Programs & Mini-Courses.
- Check Now FADIC Book store and Buy books in different specialties.
- Watch Now FADIC TV to Keep your self Updated.
- FADIC Podcast focusing on varieties of pharmacist perspectives in different specialties.
- Read more about Antimicrobial Stewardship Strategies.
- Learn More about COVID-19 info-graph, from this LINK.
- Learn More about Important Role of Pharmacist info-graph, from this LINK.
- Download Now info-graphs of Role of Pharmacist in COVID-19, from this LINK.
For further Reading about Covid-19:
- Subscribe Now in FADIC 2020 COVID19 Daily News (FNN) and Keep Updated.
- Check Now about Coronavirus Resource Information Center.
- Learn More about all What you need about Cornonavirus
- Read More about COVID 19 Patient Education from FADIC
- The Corona Virus Experimental Treatment from FADIC
- Know all What you need about Cornonavirus from Arabic Blog
- Learn More about Cornonavirus from Arabic Blog
- Medical Resources Mini-course

 Log in
Log in Sign up
Sign up