Antimicrobial Stewardship in Surgical Prophylaxis
Surgical Antimicrobial Prophylaxis and Stewardship
Author: Dr Rasha Abdelsalam Elshenawy
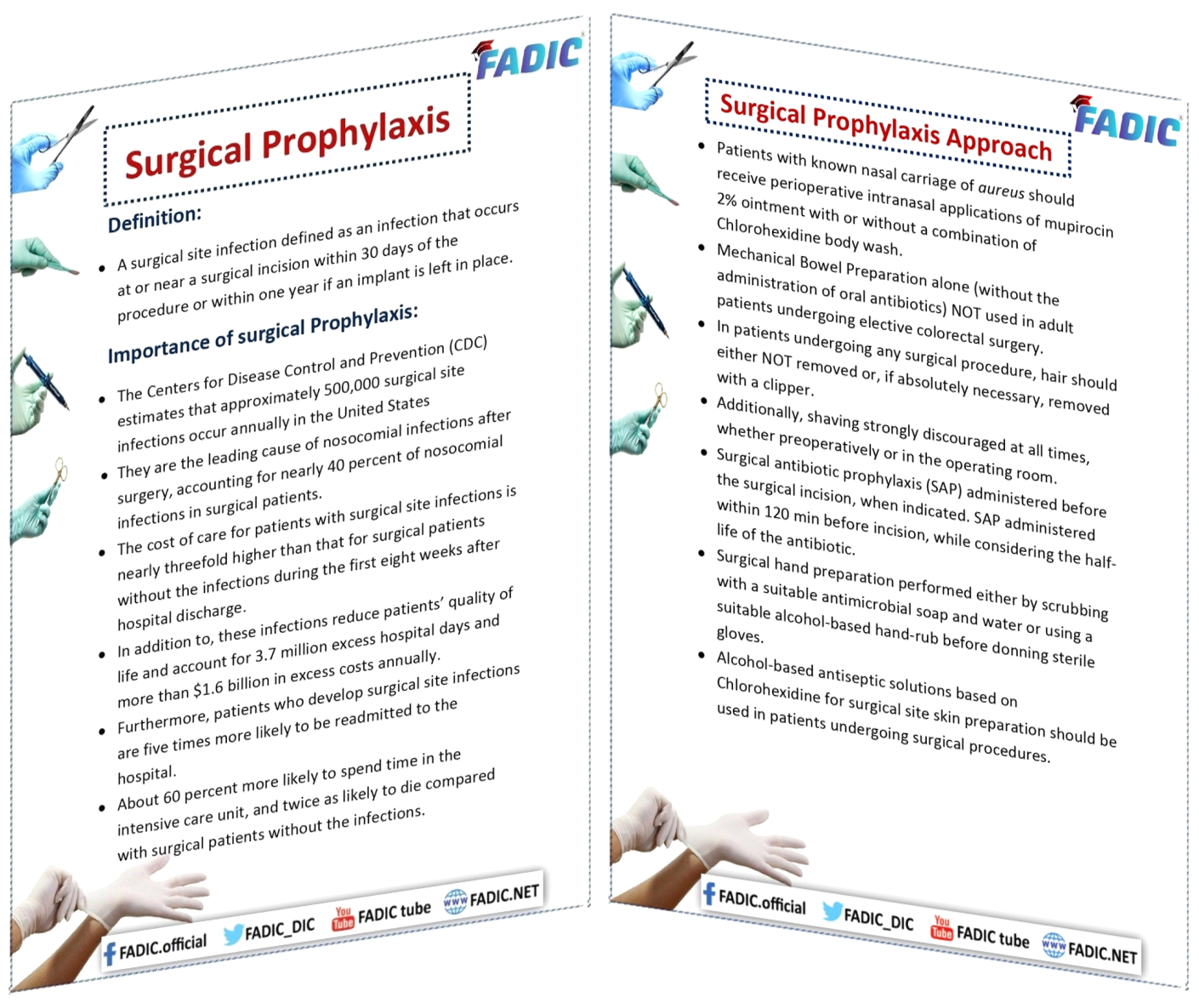
1- Importance of surgical prophylaxis:
- Antimicrobial Stewardship in Surgical Prophylaxis is one of the stewardship strategies.
- A surgical site infection is defined as at or near a surgical incision within 30 days of the procedure or one year if an implant is left in place.
- The Centers for Disease Control and Prevention (CDC) estimates that approximately 500,000 surgical site infections occur annually in the United States.
- They are the leading cause of nosocomial infections after surgery, accounting for nearly 40 per cent of nosocomial infections in surgical patients.
- The cost of care for patients with surgical site infections is nearly threefold higher than that for surgical patients without the conditions during the first eight weeks after hospital discharge.
- In addition, these infections reduce patients’ quality of life and account for 3.7 million excess hospital days and more than $1.6 billion in excess costs annually.
- Furthermore, patients who develop surgical site infections are five times more likely to be readmitted to the hospital.
- About 60 per cent more likely to spend time in the intensive care unit and twice as likely to die than surgical patients without the infections.

2- Surgical Antimicrobial Prophylaxis Approach:
Surgical Antimicrobial Prophylaxis:
- Patients with known nasal carriage of aureus should receive preoperative intranasal applications of Mupirocin 2% ointment with or without a combination of Chlorohexidine body wash.
- Mechanical Bowel Preparation alone (without the administration of oral antibiotics) is NOT used in adult patients undergoing elective colorectal surgery.
- In patients undergoing any surgical procedure, hair should either NOT be removed or, if necessary, removed with a clipper.
- Additionally, shaving is strongly discouraged at all times, preoperatively or in the operating room.
- Surgical antibiotic prophylaxis (SAP) administered before the surgical incision, when indicated.
- SAP is administered within 120 min before the incision while considering the half-life of the antibiotic.
- Surgical hand preparation performed either by scrubbing with a suitable antimicrobial soap and water or using a proper alcohol-based hand rub before donning sterile gloves.
- Alcohol-based antiseptic solutions based on Chlorohexidine for surgical site skin preparation should be used in patients undergoing surgical procedures.
Highly recommend online Marketing tool from SEMRUSH
Intra & postoperative measures:
- Adult patients undergoing general anaesthesia with endotracheal intubation for surgical procedures.
- It should receive an 80% fraction of inspired oxygen intraoperatively and, if feasible, in the immediate postoperative period for 2–6 h.
- In addition, surgical antibiotic prophylaxis administration is prolonged after the operation’s completion.
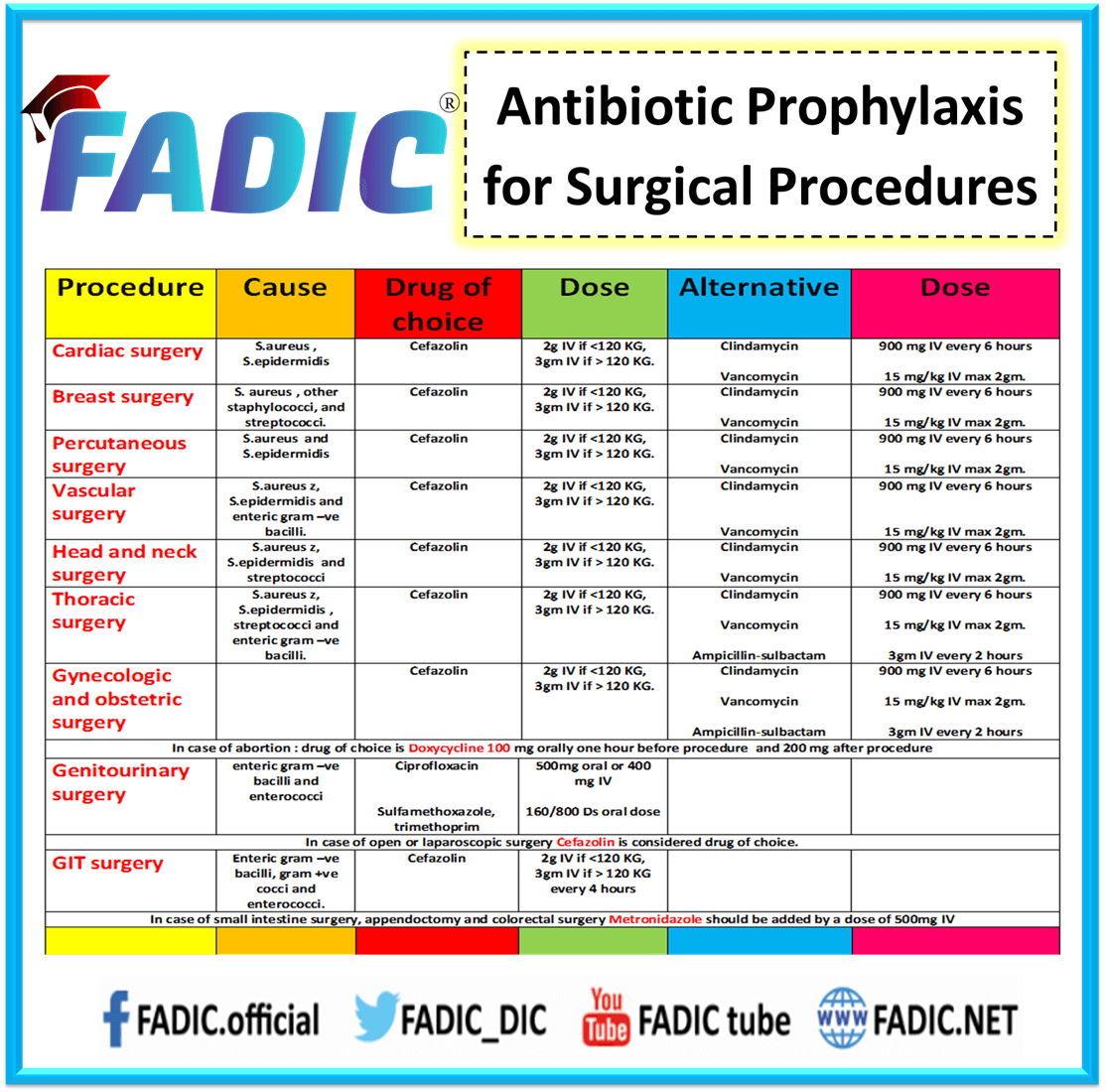
3- Surgical Antimicrobial Prophylaxis about the different procedure types:
1- Cardiac Surgery 💊
2- Breast Surgery 💊
3- Percutaneous Surgery 💊
4- Vascular Surgery 💊
5- Head and Neck Surgery 💊
6- Thoracic Surgery 💊
7- Gynecologic and Obstetric Surgery 💊
8- Genitourinary Surgery 💊
9- GIT Surgery 💊
10- Dental Surgery 💊
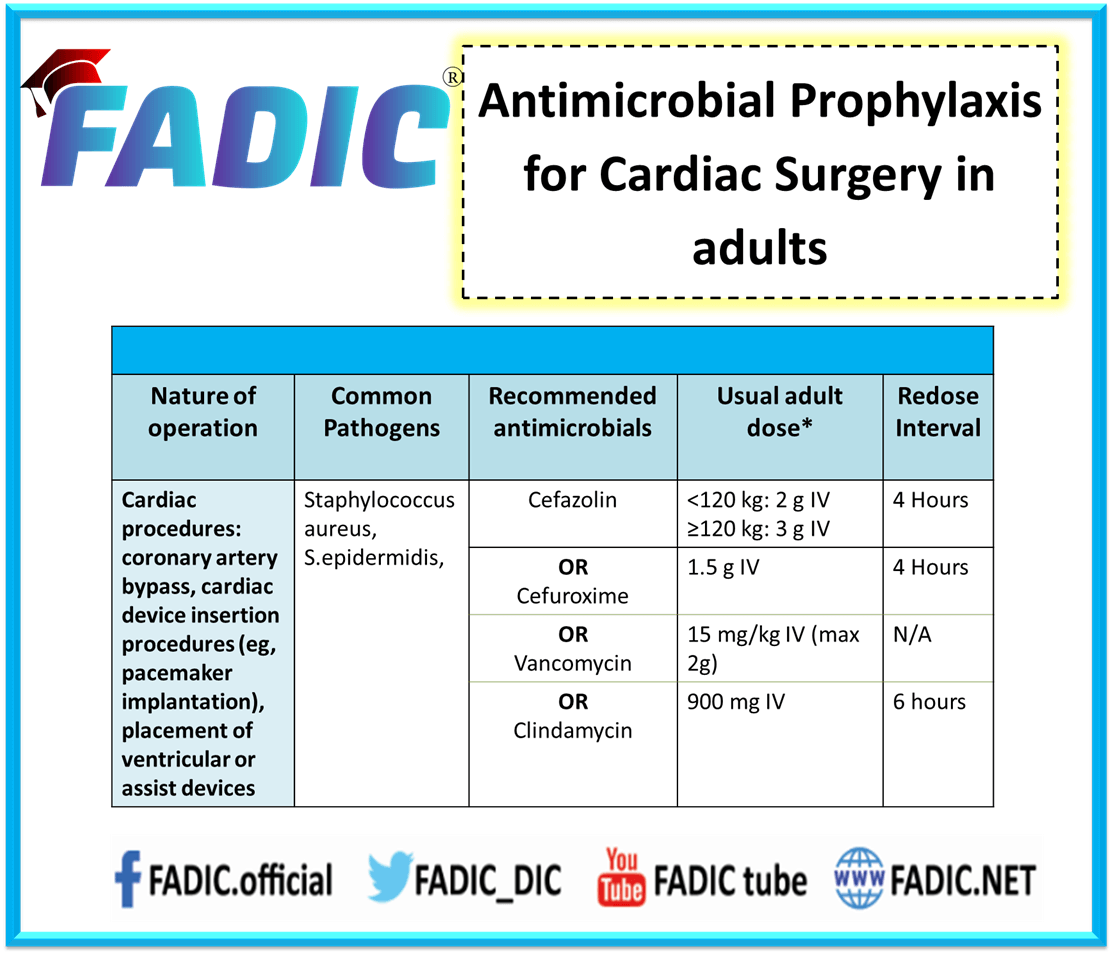
Antimicrobial prophylaxis for Cardiac Surgery
- Based on available data and perceived infection risk, antimicrobial prophylaxis is not routinely recommended for cardiac catheterisation or transesophageal echocardiogram.
- Commonly, the cause of infection is S.aureus and S.epidermidis.
- Additionally, A single dose of cefazolin or cefuroxime is recommended for device implantation or generator replacement in a permanent pacemaker,
- In addition to implantable cardioverter defibrillator or cardiac resynchronisation device.
- Clindamycin or vancomycin is an acceptable alternative in patients with a documented b-lactam allergy
- Finally, Vancomycin is considered for prophylaxis in patients known to be colonised with MRSA.
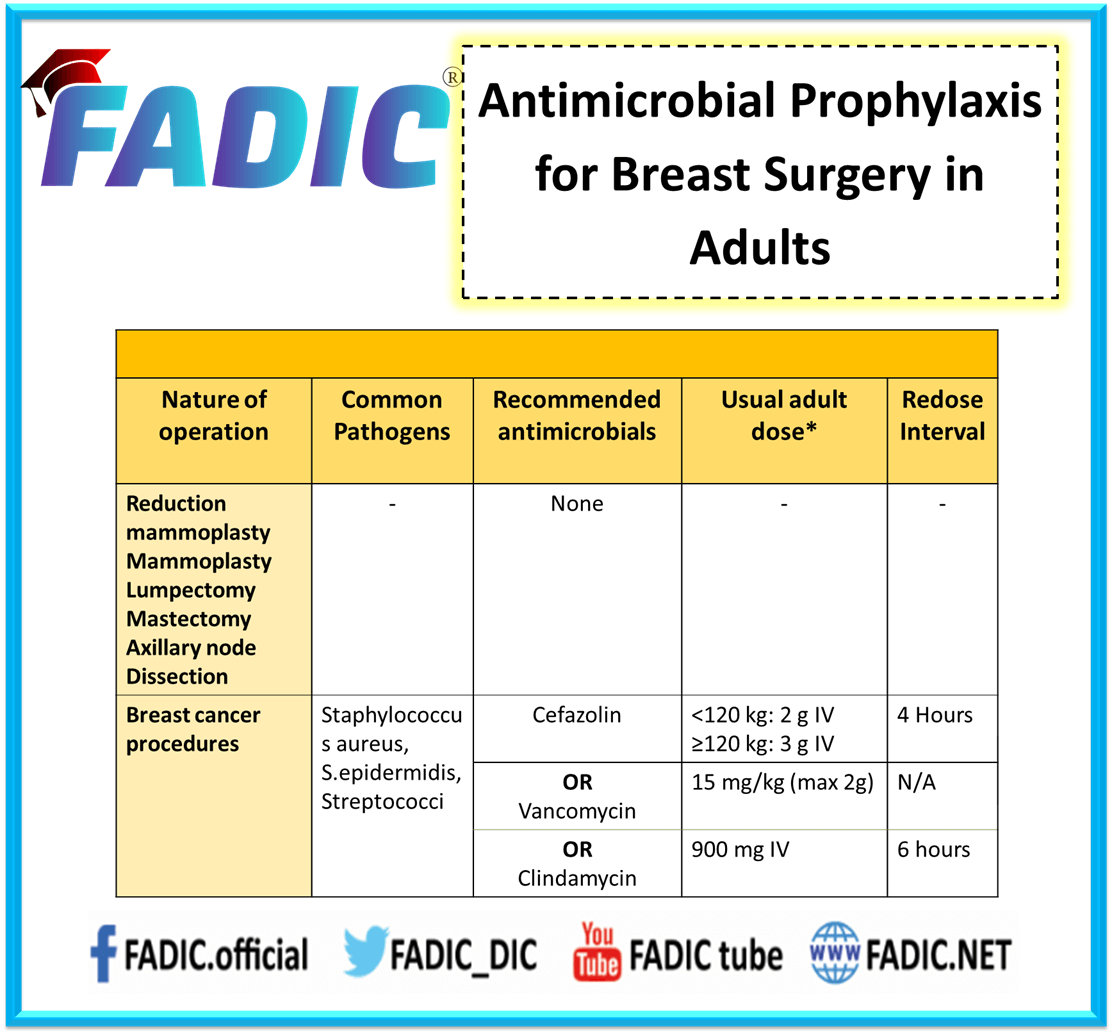
Antimicrobial Prophylaxis for Breast Surgery
The most common organisms are S. aureus, other staphylococci, and streptococci.
- Cefazolin or ampicillin–sulbactam is sufficient in most cases, with clindamycin and vancomycin as alternatives for patients with b-lactam allergy.
- Cefazolin dose is 2g IV if <120 KG, 3gm IV if > 120 KG.
- In addition, if the patient is b-lactam allergic, adding aztreonam, gentamicin, or single-dose fluoroquinolone should be considered.
- Antimicrobial prophylaxis is limited to the shortest duration possible to prevent SSIs.
Antimicrobial prophylaxis for Percutaneous Surgery
- Most common cause of infection is S.aureus and S.epidermidis.
- Routine prophylaxis is not recommended in all cases except Endograft placement.
- Drug of choice: cefazolin, followed by clindamycin and Vancomycin
- Cefazolin dose is 2g IV if <120 KG, 3gm IV if > 120 KG.
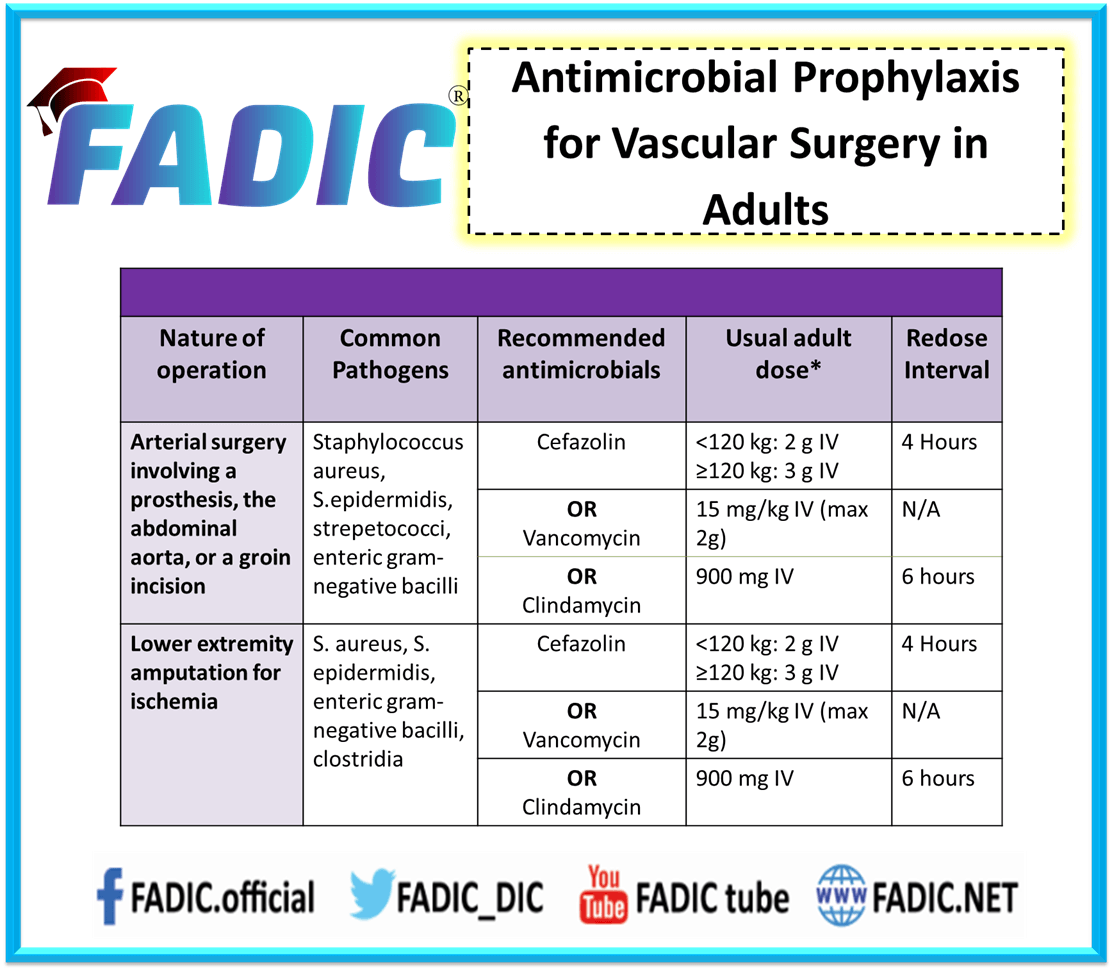
Surgical Antimicrobial Prophylaxis for Vascular Surgery
- Most common cause of infection is S.aureus z, S.epidermidis and enteric gram –ve bacilli.
- Drug of choice: cefazolin, followed by clindamycin and Vancomycin
- Cefazolin dose is 2g IV if <120 KG, 3gm IV if > 120 KG every 4 hours.
- Vancomycin 15 mg/kg IV max 2gm.
- Clindamycin 900 mg IV every 6 hours.
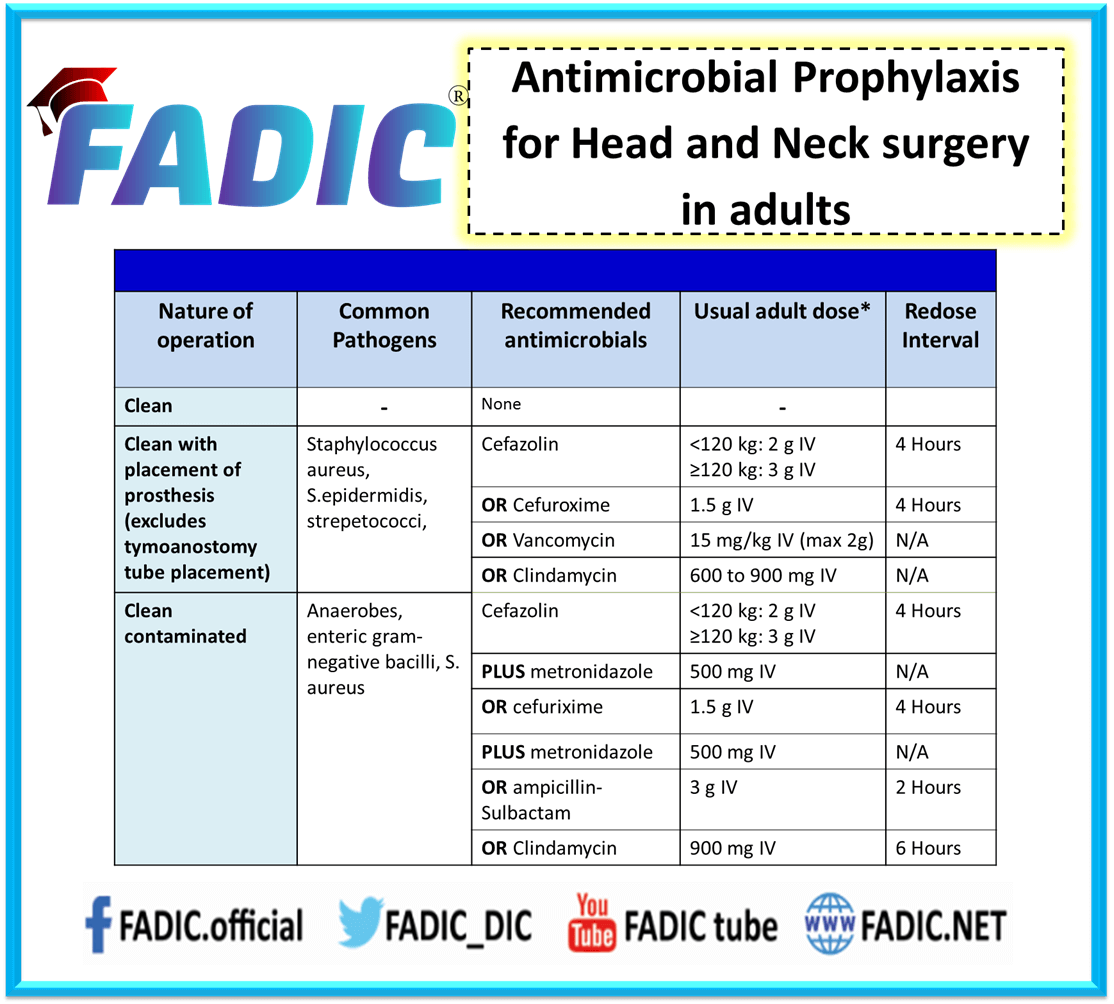
Surgical Antimicrobial Prophylaxis for Head and Neck Surgery
- Most common cause of infection is S.aureus z, S.epidermidis and streptococci
- Drug of choice is cefazolin
- Cefazolin dose is 2g IV if <120 KG, 3gm IV if > 120 KG every 4 hours.
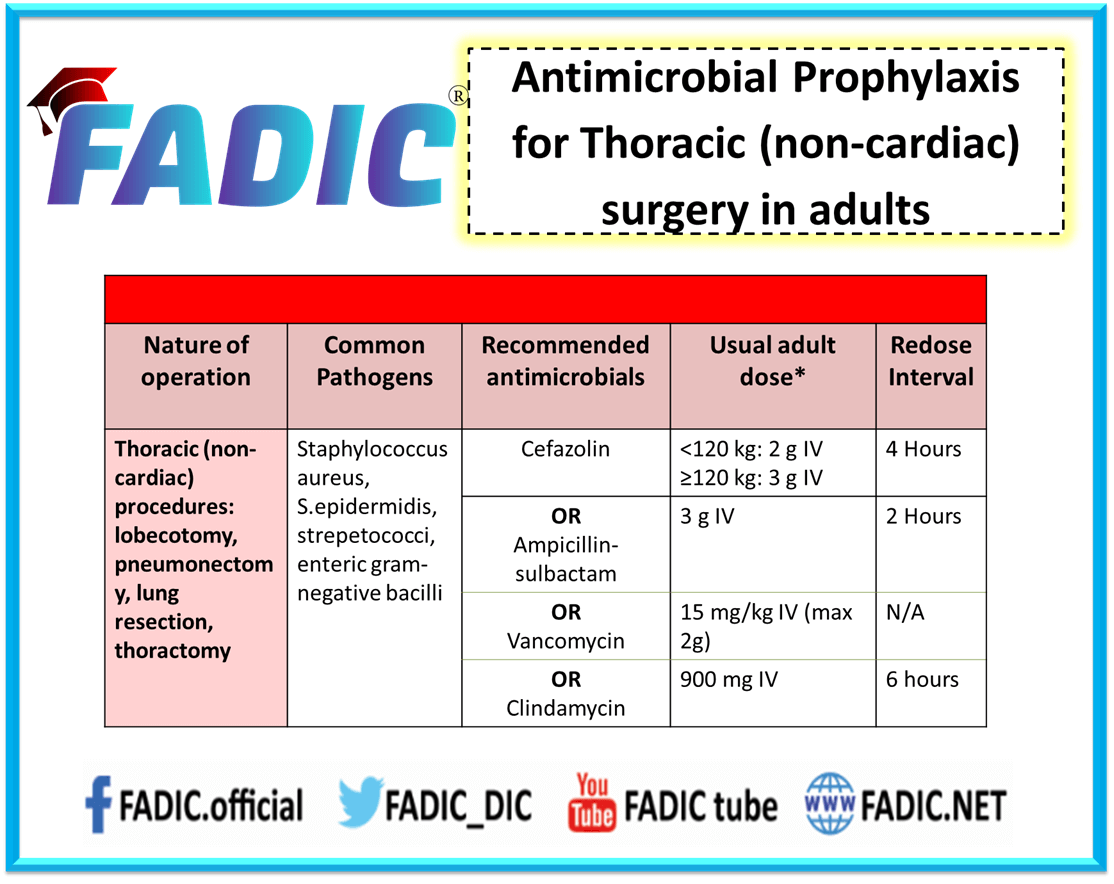
Surgical Antimicrobial Prophylaxis for Thoracic Surgery
- Most common cause of infection is S.aureus z, S.epidermidis, streptococci and enteric gram –ve bacilli.
- Drug of choice is cefazolin, ampicillin-sulbactam, clindamycin and Vancomycin
- Cefazolin dose is 2g IV if <120 KG, 3gm IV if > 120 KG every 4 hours.
- Ampicillin-sulbactam 3gm IV every 2 hours.
- Vancomycin 15 mg/kg IV max 2gm.
- Clindamycin 900 mg IV every 6 hours.
Surgical Antimicrobial Prophylaxis for Gynecologic and Obstetric Surgery
The drug of choice is cefazolin
- Ampicillin-sulbactam, clindamycin and Vancomycin are alternatives.
- Cefazolin dose is 2g IV if <120 KG, 3gm IV if > 120 KG every 4 hours.
- Ampicillin-sulbactam 3gm IV every 2 hours.
- Vancomycin 15 mg/kg IV max 2gm.
- Clindamycin 900 mg IV every 6 hours.
- In the case of abortion, the drug of choice is Doxycyclin 100mg orally one hour before and 200 mg after the procedure.
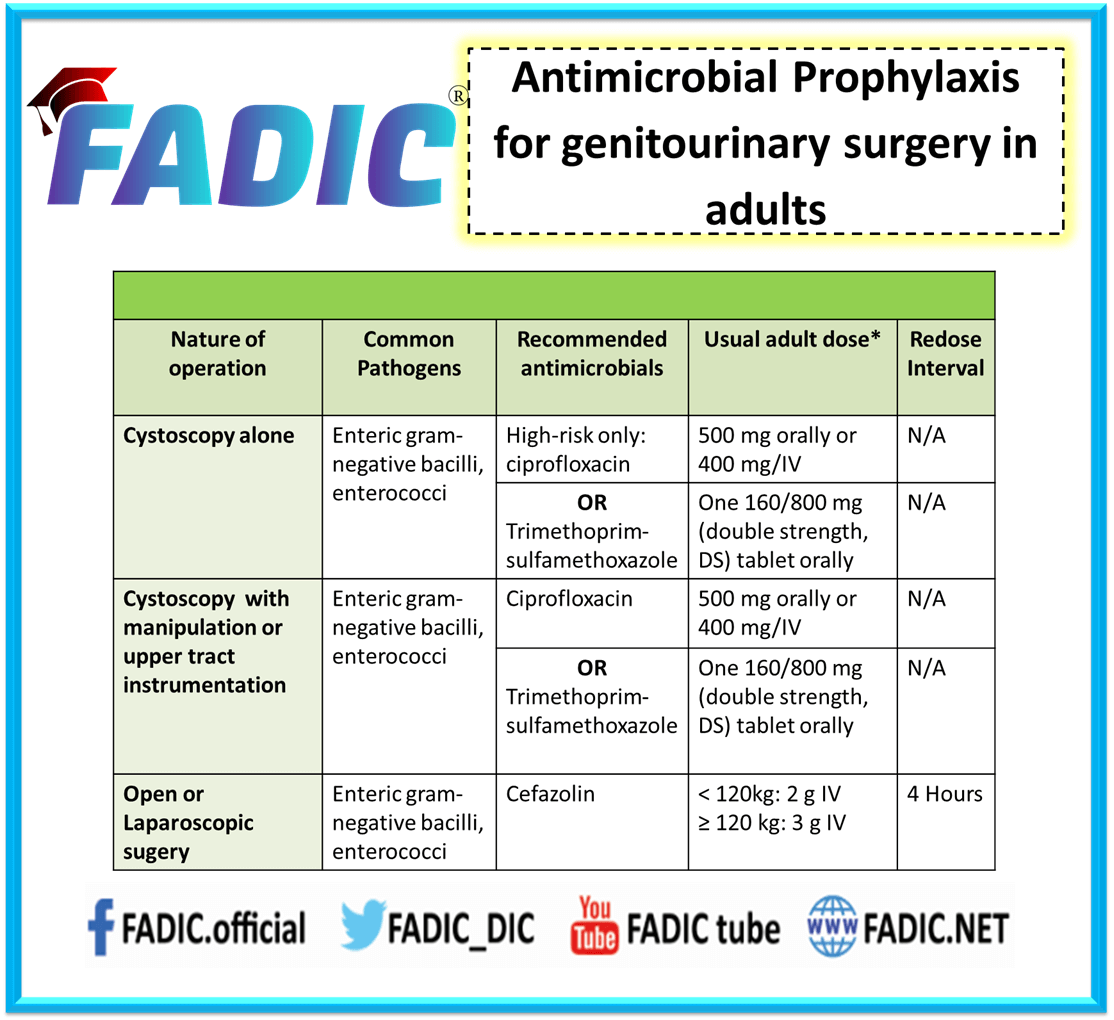
Surgical Antimicrobial Prophylaxis for Genitourinary Surgery
- Most common cause of infection is an enteric gram–bacilli and enterococci.
- Drug of choice is ciprofloxacin and sulfamethoxazole, trimethoprim
- Ciprofloxacin dose is 500mg oral or 400 mg IV
- Sulfamethoxazole, trimethoprim dose is one 160/800 Ds oral dose
- In case of open or laparoscopic surgery, cefazolin is considered the drug of choice
- Cefazolin dose is 2g IV if <120 KG, and 3gm IV if > 120 KG every 4 hours.
Surgical Antimicrobial Prophylaxis for GIT Surgery
- Most common cause of infection is an enteric gram –ve bacilli, gram +ve cocci and enterococci.
Drug of choice:
- In the case of gastroduodenal, biliary tract surgery, minor intestine surgery, appendectomy, colorectal surgery and hernia repair, it’s cefazolin
- Additionally, the Cefazolin dose is 2g IV if <120 KG, 3gm IV if > 120 KG every 4 hours.
- Furthermore, in case of minor intestine surgery, appendectomy and colorectal surgery, Metronidazole added by a dose of 500mg IV
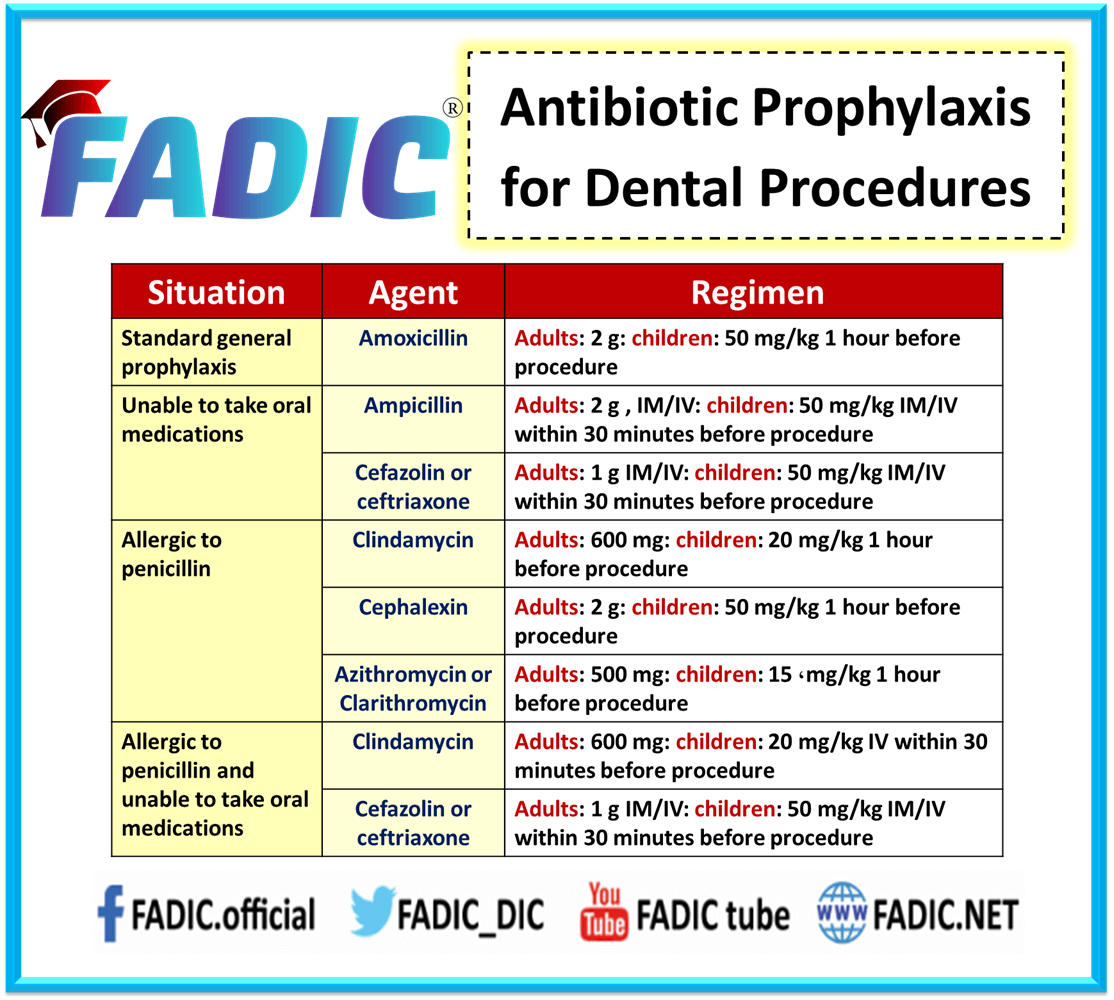
Dental Procedure Guidelines
- Antibiotics are indicated when clinical signs of involvement are evident.
- The primary use of antibiotic prophylaxis for dental procedures are cases which cause bleeding in the oral cavity.
Penicillin:
- It is the drug of choice in treating odontogenic infections as prone to gram-positive aerobes and intraoral anaerobes, organisms found in alveolar abscesses, periodontal abscesses and necrotic pulps.
- A combination of penicillin and clavulanic acid is preferred for infections caused by staphylococcus, streptococci and pneumococci.
- Patients allergic to penicillin are treated with clindamycin 300 mg (65%), which is the ideal drug of choice and followed by azithromycin(15%) and metronidazole-spiramycin(13%)
- The first-generation cephalosporins like cefadroxil and ephedrine provide a broad-spectrum antibiotic when gram-positive organisms are suspected to be the causative factor of the infection.
- Infective endocarditis is an uncommon but severe and often life-threatening condition.
- In addition, the pathogenesis of infective endocarditis comprises a complex sequence of events.
- Moreover, antibiotic prophylaxis not only acts by destroying bacteria but also by inhibiting bacterial adherence.
- Additionally, high-risk dental procedures are indicated in patients with pre-existing high-rate cardiac disorders.
- The standard regimen includes high doses of amoxicillin in children and adults one hour before the dental treatment.
- Finally, the dose is 2 g of oral amoxicillin should be given.
Surgical Antimicrobial Prophylaxis in Penicillin Allergy
- Firstly, Clindamycin is recommended in patients allergic to beta-lactams.
- In patients allergic to penicillin or amoxicillin, the first-generation oral cephalosporin is recommended.
- Additionally, Vancomycin and streptomycin are used prophylactically to prevent infective endocarditis in patients with prosthetic heart valves.
- Moreover, Antibiotic prophylaxis is advisable before invasive dental procedures as these transplant patients are more susceptible to infection.
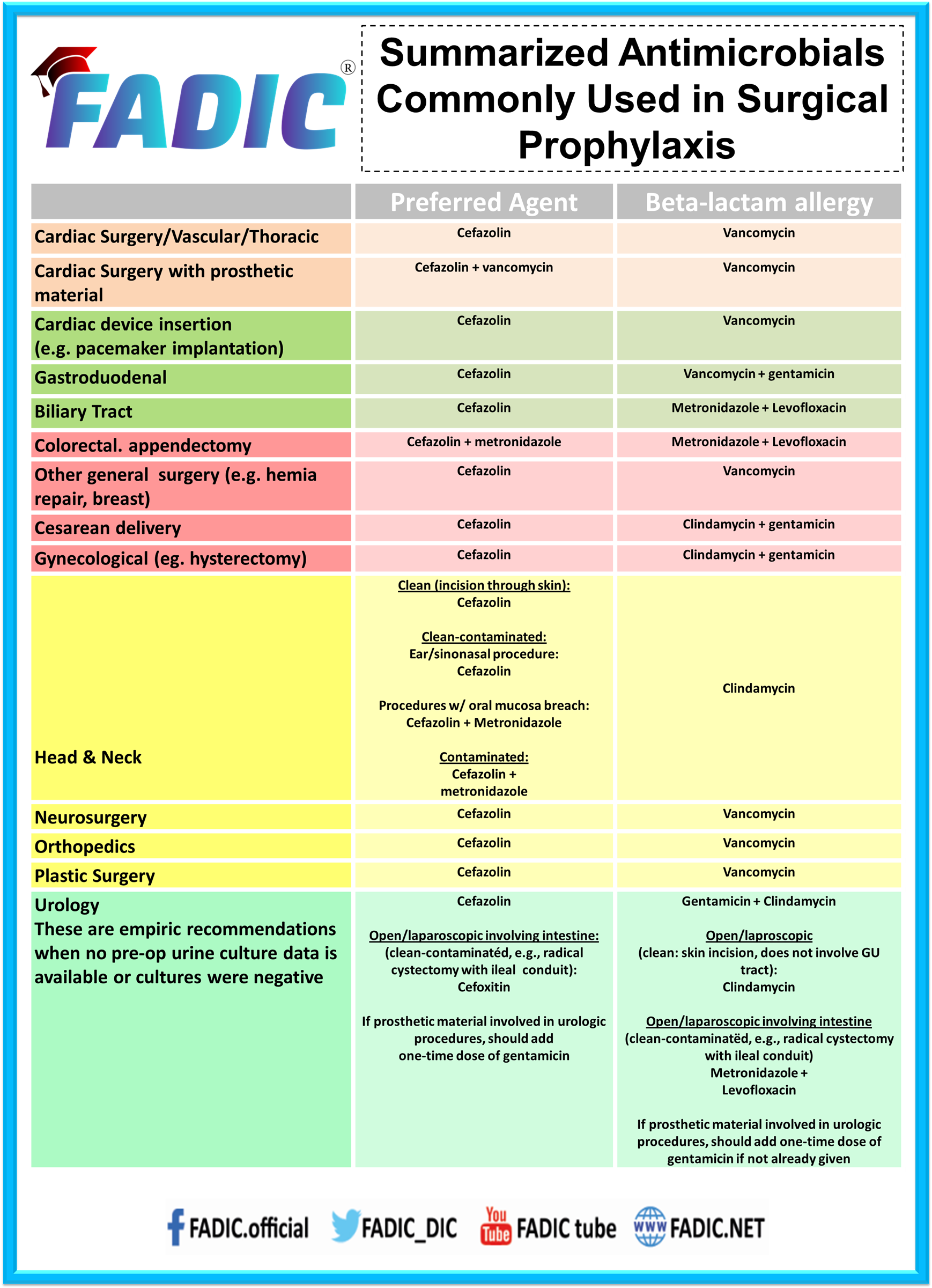
Summarised Common Surgical Antimicrobial Prophylaxis
Antimicrobial Stewardship in Surgical Prophylaxis and Surgical Site Infection
- The administration of surgical antimicrobial prophylaxis is central to preventing infection following surgery and covers breakdowns in other elements of surgical site infection prevention.
- Nonetheless, there is a growing concern for microbial resistance due to the overuse of antibiotics.
- Antibiotic stewardship programs are critical to surgical specialities due to their prominent role in prophylactic antibiotic usage and management of surgical infections.
- Moreover, such programs aim not only to reduce the development of resistant organisms.
- Additionally, ensure that misguided overuse or inappropriate use of prophylactic and therapeutic antibiotics does not harm patients.
The Following Recommendations Can Help Surgeons Incorporate Best-Evidence Practices:
- Prophylactic antibiotics are discontinued at the end of the procedure for routine general surgery cases.
- In addition, Prolonged use—even for only 24 hours—does not help prevent surgical site infections.
- Topical antibiotics not indicated in the era of prophylactic systemic antibiotic therapy.
- A meta-analysis comparing appendectomy and colorectal surgery patients with and without systemic antibiotic prophylaxis demonstrated that topical antibiotics’ surgical site infection benefit disappeared when using routine, prophylactic systemic antibiotics.
- Limited, fixed courses of antibiotics are sufficient for treating complex intra-abdominal infections after controlling the infectious source.
- Additionally, Incision and drainage of superficial skin abscesses and opening of infected superficial surgical site infections is an effective treatment.
- Moreover, Antibiotic treatment is not necessary after appropriate drainage.
- Then, Uncomplicated diverticulitis does not typically treat with antibiotics.
- Asymptomatic bacteriuria is distinguished from urinary tract infections, and the former is not treated with antibiotics except for pregnant women and men with prostate resections.
Conclusion
- In conclusion, surgical site infection is defined as an infection that occurs at or near a surgical incision within 30 days of the procedure.
- Finally, The administration of antimicrobial agents is central to preventing infection following surgery and covers unrecognised breakdowns in other elements of surgical site infection prevention.
- This is Antimicrobial Stewardship in Surgical Prophylaxis
Join Surgical Prophylaxis Antimicrobial Stewardship Course to learn how to apply stewardship in surgery

 Log in
Log in Sign up
Sign up