FADIC Guide for Travel Medicine
Travel medicine is an interdisciplinary speciality devoted to the health of travellers who visit foreign countries.
Travel medicine is concerned explicitly with preventing infectious diseases during travel.
It’s also concerned with ensuring the personal safety of travellers and avoiding environmental risks.
Globalisation facilitates the spread of disease and increases the number of travellers exposed to a different health environment.
The field of travel medicine encompasses a wide variety of disciplines, including
- Epidemiology
- infectious disease
- public health
- tropical medicine
- high altitude physiology
- travel-related obstetrics
- psychiatry
- occupational medicine
- military and migration medicine
- environmental health
Highly recommend online Marketing tool from SEMRUSH
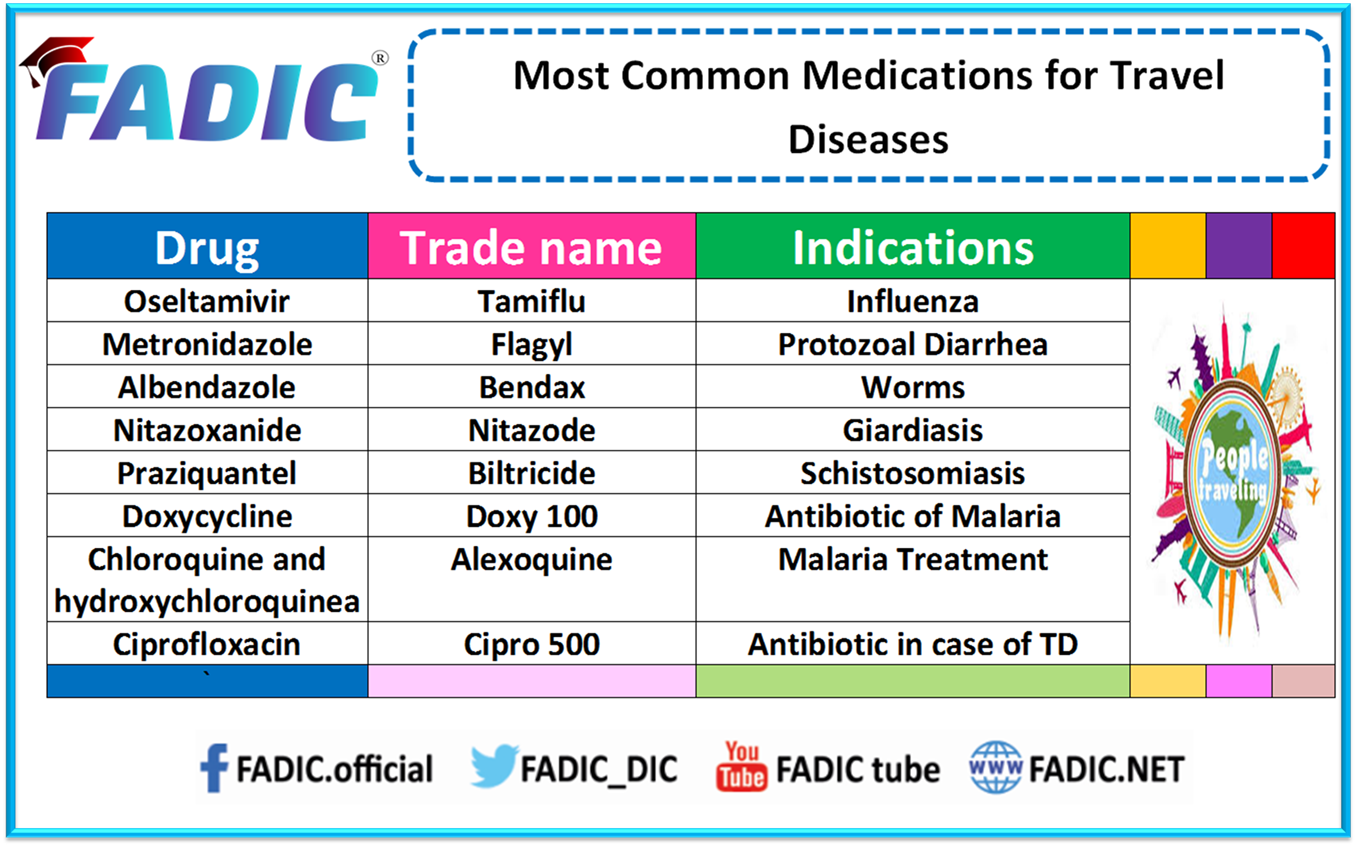
Most Common Medications for Travel Diseases
Most standard travel diseases and their treatment:
MALARIA
Malaria is one of the most severe infectious diseases among travellers,
However, almost all travel-related cases are preventable.
The disease is caused by Plasmodium spp., a parasitic protozoan transmitted by female Anopheles mosquitoes.
This mosquito is unique because it is a rural night biter.
Malaria is a tremendous public health problem because more than 40% of the world’s population is at risk.
Malaria is endemic in tropical and subtropical areas of Africa, South America, Asia, and Oceania.
Symptoms:
- shaking chills that can range from moderate to severe
- high fever
- profuse sweating
- headache
- nausea
- vomiting
- abdominal pain
- diarrhoea
- anaemia
- muscle pain
- convulsions
- coma
- bloody stools
Prevention:
- Travel to malarious areas should be discussed in the pretravel assessment
- Bed nets should be used in addition to repellants and
Protective clothing:
- Travelers should be adherent to their antimalarial regimen.
- Travelers should be encouraged to seek medical attention should fever develop during travel
Chemoprophylaxis for Malaria:
Chloroquine and hydroxyl chloroquine: Start 1–2 wk before travel; continue weekly during and 4 wk after returning
Doxycycline: Start 1–2 days before the trip; continue daily during and 4 wk after returning
Primaquine: Start 1–2 days before the trip; continue daily during and 1 wk after returning
Treatment Options:
- Plaquenil:
620 mg base (= 800 mg of salt) PO immediately, followed by 310 mg base (= 400 mg of salt) PO at 6, 24, and 48 hr
Quinine dihydrochloride:
20 mg of salt/kg loading dose infused during 4 hr, followed by maintenance of 10 mg of salt/kg infused over 3–4 hr every 8 hr
Oral therapy can be used to complete a 7-day course (quinine sulfate plus doxycycline
Quinidine gluconate plus doxycycline, tetracycline or clindamycin:
10 mg of salt/kg IV infused over 1–2 hr, followed by a continuous infusion of 0.02 mg of salt/kg/min for at least 24 hr and then until parasitemia < 1%
Doxycycline 100 mg IV/PO twice daily
Tetracycline 250 mg PO four times daily
Clindamycin 20 mg base/kg/day PO divided over three times daily
Clindamycin IV dosing is 10 mg base/kg, followed by 5 mg base/kg three times daily
Traveller’s Diarrhea
TD is the most common illness in individuals travelling from resource-rich to resource-limited regions.
TD is caused by ingesting contaminated food and beverage.
More than 90% will consume unsafe food and drink within days of arriving at their destinations.
Symptoms of TD may resemble or overlap with “food poisoning.”
The aetiology of the disease is determined by geography and can affect the therapy selection.
Of the bacterial causes, enterotoxigenic E. coli is the most common pathogen.
Prevention:
- Avoiding foods that travellers cannot boil, cook, or peel themselves
- avoidance of the following:
- Tap water (including food washed in water)
- Unpasteurized milk
- Salsas
- Raw or undercooked meats
- hand washing or use of alcohol-based sanitisers
- receipt of vaccines that can prevent food- and waterborne infection. Od from street vendors
Chemoprophylaxis for TD:
1- Bismuth subsalicylate: 2 tablets chewed every 6 hr
2- Ciprofloxacin: 500 mg once or twice daily
Treatment:
1- Bismuth subsalicylate: 2 tablets chewed every 6 hr
2- Loperamide: 4 mg initially; then 2 mg after each unformed stool
3-Short-course antimicrobial therapy (1–3 days) is often effective and decreases the duration of illness to about 1½ days
Ciprofloxacin: 500–750 mg daily for 1–3 days
4- Treatment options for protozoal pathogens include
- Tinidazole
- Metronidazole
- Nitazoxanide
Viral Infections
1- Zika Virus
First mosquito-borne virus with the capacity for sexual transmission.
Flavivirus is closely related to dengue, yellow fever, Japanese encephalitis, and West Nile viruses.
Methods of transmission
- Mosquito bite
- Blood transfusion
- Percutaneous
- Sexual contact
- Intrauterine
- Intrapartum from a viremic mother to newborn
Symptoms:
- Rash (maculopapular; often pruritic(
- Fever (usually low grade/short term(
- Arthritis, myalgias, and arthralgias
- Nonpurulent conjunctivitis
Treatment:
Treatment should focus on preventive efforts, including preventing further transmission, employing vector control, and avoiding mosquito bites with repellants.
Currently, no antiviral agent with appreciable activity exists, and supportive care is recommended.
2- Ebola Virus
Belongs to the family Filoviridae, closely related to the Marburg virus.
There are five species of Ebola virus, all of which cause human disease except for R. ebolavirus.
Methods of transmission:
- Contact a reservoir host
- Person-to-person transmission through blood or body fluids poses the highest risk of transmission.
Symptoms:
- Fever (80% of patients)
- Severe headache
- Fatigue740
- Myalgia
- Vomiting/diarrhoea
- Abdominal pain
- Elevated liver function tests
- Renal failure
- Blood dyscrasias (leukopenia/thrombocytopenia)
Treatment:
There is no known treatment, and care is mainly supportive, including:
- Intravenous fluid resuscitation is considered critical in treating patients.
- Electrolyte replacement
- Empiric antibiotics and/or antimalarials
- Respiratory supportive care
3- Dengue
Most common arbovirus infecting humans.
Vectors are A. aegypti and A. albopictus.
Considered endemic in over 100 countries, resulting in an estimated 50 million infections annually.
Increased global travel, urban crowding, and ineffective mosquito control have allowed dengue to become a pandemic.
Transmitted predominantly through mosquitos.
Symptoms:
- can be asymptomatic or subclinical.
- Often characterised by a febrile state called (breakbone fever)
- Typical incubation period is 3–14 days with symptoms following three phases:
- Initial febrile phase
- Characterized by high temperature with headache, myalgias, vomiting, and joint pain
- Resolution is typically 3–7 days later, and most patients recover without further sequelae.
5. Critical phase
- typically occurs around the time of defervescence
- Clinicians should be aware of this phase because patients can rapidly deteriorate to dengue shock syndrome.
- Early signals of possible significant vascular leakage include major skin bleeding, high or increasing hematocrit with a concurrent decrease in platelet counts, lethargy, and restlessness.
- Signs and symptoms consistent with disseminated intravascular coagulation can also be present in this phase.
6. Spontaneous recovery/convalescent phase
- The vascular leak reverts after 48–72 hours and is associated with improved patient symptoms.
- A maculopapular rash may also be present during this phase
Treatment:
- Supportive care is the cornerstone of treatment.
- Fluid management is imperative.
- No antiviral agents with appreciable activity are currently available.
- Other therapies that have been investigated include:
- Doxycycline
- Pentoxifylline
- Celgosivir
- Ivermectin
4- West Nile Virus
Second-most common flavivirus infection only to dengue.
Methods of transmission:
- Transmission is optimal during the summer months.
- Warmer temperatures foster infectivity and transmission efficiency.
- Transmission occurs almost exclusively by the Culex mosquito
Symptoms:
- Headache
- Myalgia
- Maculopapular or morbilliform nonpruritic rash
- Recovery often takes weeks to months.
- Up to 50% who develop West Nile neuroinvasive disease have functional and/or cognitive sequelae, particularly with encephalitis.
Treatment:
- Preventive strategies, including vector control and use of insect repellants
- Management is largely considered supportive
Travel- Borne Rickettsioses
Rickettsioses are obligate intracellular pathogens, with many arthropods serving as competent vectors.
These include lice, fleas, ticks, and mites.
Rickettsioses are divided into three groups:
- two diseases in the typhus group
- 15 diseases in the spotted fever group
- one disease in the scrub typhus group
1- Murine Typhus
Also called “endemic typhus” or “flea-borne typhus.”
Rodents and rat fleas serve as the primary vector(s), with endemicity linked to high rat (rodent)
Transmission is closely correlated with fleas versus rodent reservoirs.
Infection often occurs without recognised contact with fleas or associated vectors.
Symptoms:
- Nonspecific, with fever and maculopapular rash as the most common features
- Incubation period is 7–14 days.749
- The rash may be faint or absent in some patients and characteristically spares the palms and soles.
- Most disease is benign and self-limited
Treatment:
- doxycycline 100 mg twice daily is the treatment of choice in children and non-pregnant females.
- Fluoroquinolones and chloramphenicol are alternatives
2- African Tick Bite Fever
Caused by R. africae and found in almost all countries in sub-Saharan Africa and parts of the eastern Caribbean
Closely related to the Mediterranean spotted fever but does not typically cause severe illness.
Considered the most commonly encountered rickettsial infection in travel medicine
Not fully realised in travellers because of the self-limited nature of the disease.
Symptoms:
- Headache
- neck pain
- myalgia
- Eschar and localised lymphadenitis
Treatment:
- Doxycycline 100 mg twice daily for 5–7 days
- Azithromycin and fluoroquinolones are suitable alternatives
3- Mediterranean Spotted Fever
Dog ticks are the principal vectors and reservoirs for the Mediterranean spotted fever and its variants.
Endemic to the “Mediterranean area” of Europe, Africa, and Asia
Transmission is influenced by season (increased transmission in warmer months)
Warmer months increase the tendency of ticks to bite humans
Symptoms:
- Incubation period is about six days.
- Disease is very similar to African tick bite fever, with fever, maculopapular rash, and black eschar (tache noire) at the site of the tick bite as the most common symptoms.
Treatment:
Doxycycline is the treatment of choice
4- Scrub Typhus
Mite serves as the principal vector and reservoir
Transmitted by the bite of larval trombiculid mites
Associated with travel that includes trekking or camping in rural areas
Scrub typhus is a significant cause of fever in travellers returning from Asia because it is considered predominant.
Symptoms:
- Incubation period is typically 7–10 days but may extend to around three weeks.
- Lymphohistiocytic vasculitis is pathognomonic for scrub typhus
- Can be clinically challenging to differentiate from other diseases
Treatment:
- Doxycycline is considered the drug of choice, with azithromycin an alternative.
- Treatment should consist of at least three days with doxycycline.
- Rifampin as monotherapy is also an alternative regimen.
Immunisation Considerations in Travelers
The CDC and the WHO provides information about vaccines when travelling abroad.
The CDC stratifies vaccines into the following categories:
- All travellers
- Most travellers
- Some travellers
Vaccination Required Before Travelling to Specific Countries
Additional vaccination choice depends on the following:
- Region(s) visited within a given country
- Planned activities
- Duration of stay
- Time of the year
Routine Vaccines include:
- Influenza
- Td (tetanus and diphtheria)
- Tdap (tetanus, diphtheria, and pertussis)
- HPV (human papillomavirus)
- HZV (herpes zoster)
- MMR
- Hib (Haemophilus influenzae type b)
- Pneumococcal
- HAV (Havrix, Vaqta, and Twinrix)
- Hepatitis B (Engerix-B, Recombivax HB, and Twinrix)
- Japanese encephalitis (Ixiaro)
- Meningococcal (Menactra and Menomune)
- Polio (Ipol)
- Rabies (Imovax and RabAvert)
- Typhoid (Typhim Vi and Vivotif)
- Yellow fever (YF-Vax)
FAQs about travel:
What should you do with your medicines and medical supply if you are flying?
- Show your medicines to a security person
- Ask for inspection by a person, not an Xray machine
- Keep your medication in your carry-on bags so you would have them on the plane
When should I take my medicines if you are changing the time zone?
Talk to your doctor before you travel to work out a travel action plan for you.
How should you reserve your medications if you go to a hot place?
Keep your medicine in a cool, dry place.
Never keep them in the car, bathroom, or in direct sunlight.
How can you avoid blood clots if you often go on long flights?
- Walk around every hour during your flight
- Bend and straighten your legs every half an hour during your flight
- Wear compression stockings
- Avoid dehydration by drinking plenty of water
- Avoid taking sleeping tablets because they prevent you from walking around
Before you travel:
- Find out if you need travel vaccines and ensure your vaccinations are up-to-date.
- If malaria is a risk, you may need to start treatment before travelling.
- Prepare a kit of travel health essentials, including sunscreen, painkillers and antiseptic.
- Keep your medicine in your carry-on bag so you can get to your medicine during your flight
- If you have an ongoing health concern, talk to your healthcare provider about your trip.
- If you are changing time zone, talk to your doctor to work out a travel action plan for when you should take your medicine
- If you are going somewhere with hot and sticky weather, keep your medication in a cool, dry place
- Ask your doctor for a letter stating your medical history and prescribed medications.
- Carry a medical aid kit with medications and other supplies you need for your trip
- To prevent deep venous thrombosis, if you are going to be on a long flight, walk around every hour or so during your flight and try to wear compressing stockings or flight socks.
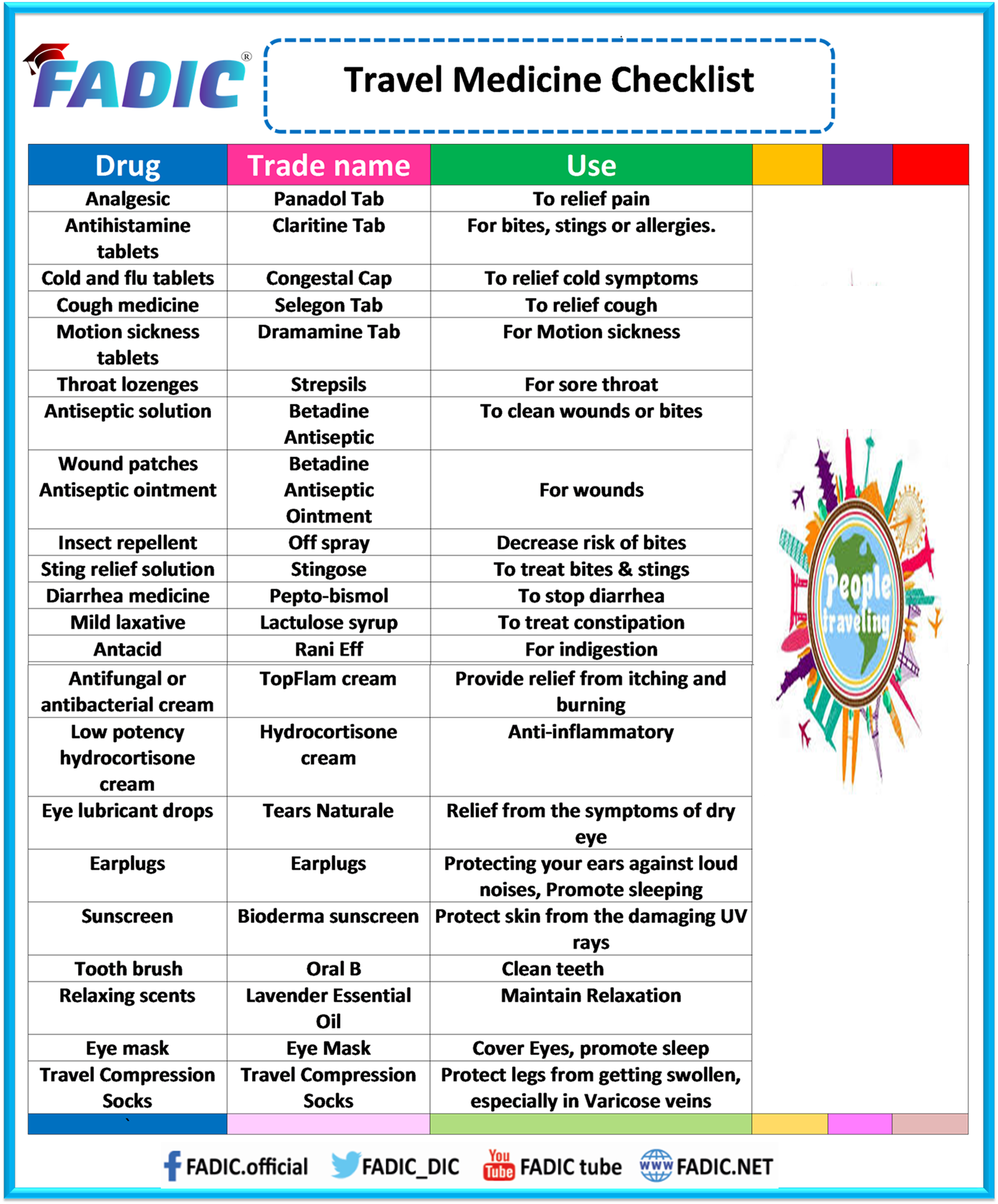
Travel Medicine Checklist
Summary:
Travel medicine is concerned explicitly with preventing infectious diseases during travel.
Before travelling, ensure you take the vaccination for the destination country.
Avoid any raw, unwashed or non-boiled food.
If you have an ongoing health concern, talk to your healthcare provider about your trip.
Read More:
- Antimicrobial Stewardship School
- Sepsis Training Program
- Download Pocket Guide for Antibiotic Pharmacotherapy Book
- Microbiology Course | ABC Bacteria
- Infectious Disease E-News | FREE Subscription
- ABC antimicrobials | Know all about the Antimicrobials
- Road Map to Antimicrobial Stewardship Training Program
- Register Now in FADIC Clinical Research School
- FADIC Drug Information Fellowship
- Buy FADIC Toolkit for Writing Research to Write a Great Research Paper
- Read 10 Skills You Must Learn to Do a Research via Google Scholar in Arabic
- The FADIC Online Continuous Medical Improvement Programs & Mini-Courses.
- Check Now FADIC Book store and Buy books in different specialities.
- Watch Now FADIC TV to Keep yourself Updated.
- FADIC Podcast focuses on varieties of pharmacist perspectives in different specialities.
- Subscribe Now to FADIC 2020 Daily News (FNN) and Keep Updated.
- Check Now about Coronavirus Resource Information Center.

 Log in
Log in Sign up
Sign up