FADIC Pharmacy Vision 2030 “Efficient Pharmacy Practice”
Why 2030 Vision?
- All success stories start with a vision, and strong visions based on active initiates, and projects.
- A vision statement is an aspirational statement of where to want to be in the future.
- It should set the overall direction for the organizations and teams.
- Moreover, it needs to be bold and inspirational.
➡ ➡ If you Don’t have time to Read, You can Download the Whole 2030 Vision from Below ➡ ➡
2018 Author of Paper
The Evaluation of Pharmacy Strategic Plan in Past 2013-2016 and Forecasting of New Vision 2030 at the Ministry of Health in Saudi Arabia
Dr. Rasha Abdelsalam
The previous vision prepared by using several tools to follow up the implantation of the strategic plan of Varies National and International Organizations such as:
- ACCP
- ASHP
- MOH
- UK- Royal Society
- Gulf Strategic Plan
- Middle East
Vision #1: Medication Information
“Every Pharmacist Should be a Trusted Drug Information Resources”
For every pharmacist working in the drug information, you should learn how to understand the question properly.
Pharmacists have traditionally played an important role as disseminators of drug information.1,2 The need to provide accurate, unbiased.
Up-to-date drug information is becoming ever more important in a world which is experiencing a drug and health information explosion.
The pharmacist still remains the most easily accessible health care professional to the general public as well as the medical community.
Therefore, more likely to be the first person approached for drug information. The pharmacists’ educational training should, theoretically, make him or her the most qualified member of the health care team to perform this duty.
PICO Questions !!!
Tips for Framing the PICO Questions

Then, search in the resources in a proper way, to know how to obtain the write, and trusted information.
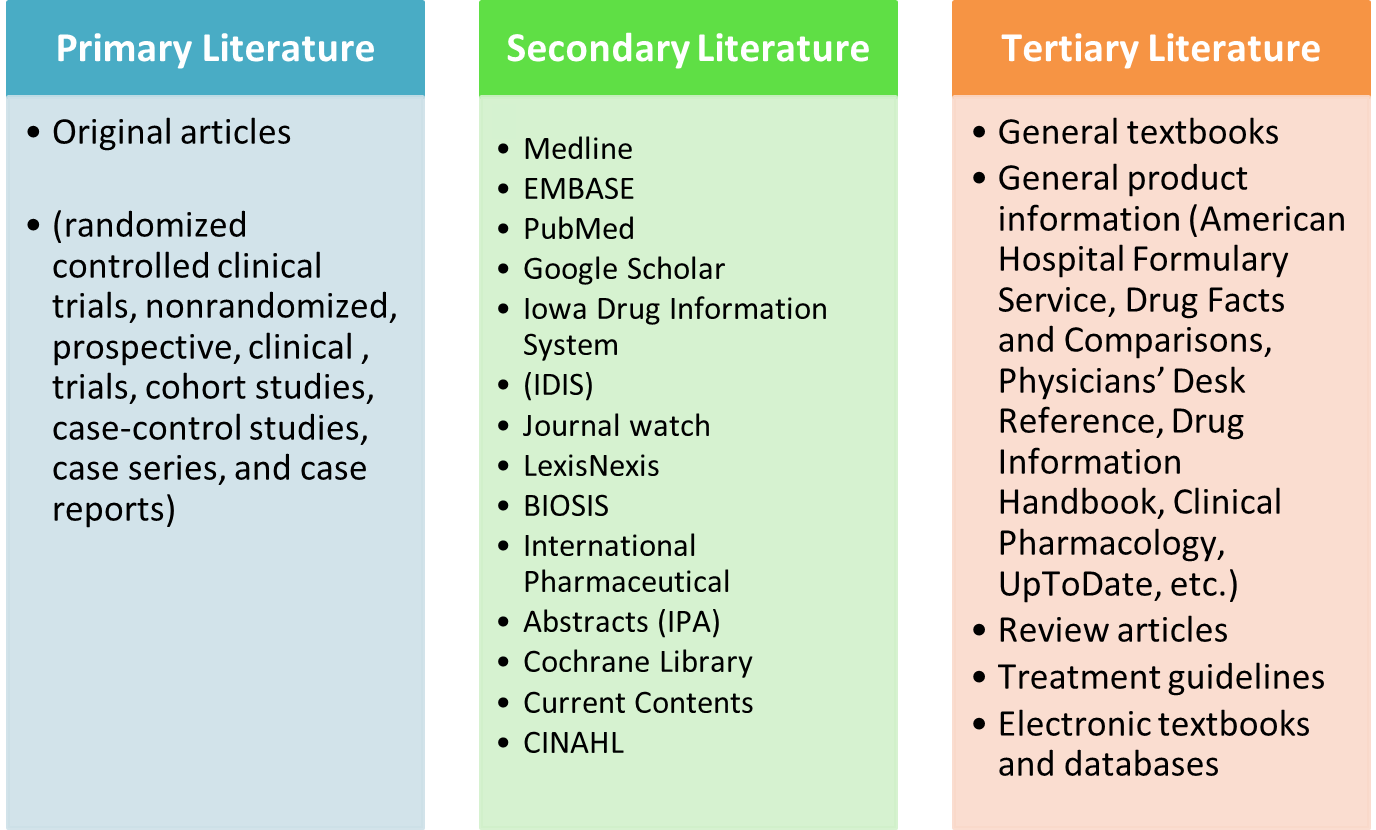
The best method to find information includes a stepwise approach moving from:
- Tertiary (e.g., textbooks, full-text, review articles)
- Then, Secondary (e.g., indexing or abstracting services )
- Finally, primary (e.g., clinical studies ) literature
The tertiary sources provide the practitioner with general information needed to familiarize the reader with the topic.
Understand the Stepwise Approach For Moving from Medical Resources
Important Advise for Every Pharmacist:
- You should know how you search for trusted information.
- The source of Information for the patient is totally different from the resources needed to search for information for healthcare professionals.
- Drug Information pharmacists need to measure their work, DAILY Workload Statistics for Drug Information on daily basis.
- In addition to MONTHLY Workload Statistics for Drug Information Pharmacists should be done to manage your work effectively.
“Join FADIC Drug Information Program will help you to understand all types of resources. You will be able to know the internet and electronic resources of the drug information.
At the end of the DIC program, you will be able to find the right information from the trusted resources. By the end of the program, you will be able to present the final journal presentation.”
Vision #2: Evidence-Based Practice
“Every Pharmacist Should Learn How to Work with an Evidence-Based Practice”
General Stepwise Approach
The best method to find information includes a stepwise approach moving from:
- Tertiary (e.g., textbooks, full-text, review articles)
- Then Secondary (e.g., indexing or abstracting services )
- Finally primary (e.g., clinical studies ) literature.
The tertiary sources provide the practitioner with general information needed to familiarize the reader with the topic.
Case Study
While searching for Information on a specific medication you find an electronic document describing a clinical experience of a practitioner with a patient who had an adverse reaction to a medication.
What kind of literature is this?
- Primary
- Secondary
- Tertiary
“Learn the EBM Tools that help you to maintain Evidence-Based Practice”
- Evidence-based medicine (EBM) is the conscientious, explicit, judicious and reasonable use of modern, best evidence in making decisions about the care of individual patients.
- EBM integrates clinical experience and patient values with the best available research information.
The Question Here: Is Evidence-Based Medicine New?

FADIC PICO Search Worksheet Book: FADIC PICO “Worksheet”
In FADIC EBM Program, You will receive your issue of the EBM worksheet Booklet to learn how to use the PICO.
This is to clearly articulate a sample clinical question. In addition, constructing and revising a PubMed.
This will help you to find the evidence-based information, that can be used in the clinical practice, research, articles, presentations.
The most important use for FADIC PICO Worksheet Booklet is to help you to share the trusted clinical information, especially in social media platforms, such as Twitter, Facebook, Blogs, and others.

PICO Search Worksheets Book
PICO Worksheet and Search Strategy Booklet from FADIC has the important principles of the forward clinical questions.
You can Define your question using PICO: Population, Intervention, Comparison, and Outcome.

Inspiring Future Quotes !!
“With increase the social media, and different internet resources. You need to learn how to find evidence-based information, from the trusted resources”
Dr Rasha Abdelsalam
Vision #3: Clinical Case Presentation
“Every pharmacist Should Learn the Guidelines for Clinical Case Presentation”
Updated Pharmacists, Education, and Research create an effective clinical practice
- The pharmacist should learn how to Maintain an effective clinical practice
- Guidelines for Clinical Case Presentation should be discussed with healthcare professionals
- Pharmacotherapy Case Reasoning is important to understand patient medications properly.
This Theme of “I am a pharmacist”
- This Call the need for expanding pharmacists role as the health care system changes?
- Need to know exactly how to differentiate a pharmacy role from a medical role?
Now asking an important question ?? What are Practices Opportunities for Pharmacists ??
The Answer is:The pharmacy profession is very promising and has the potential for optimization at an international level
However, there are some considerations that should be borne in mind in future:
-
- Harmonization of professional standards of practice is necessary and should be performed promptly and systematically.
- Appropriate distribution of pharmacists in healthcare sectors should also be considered
- Pharmacy education is currently a matter of great interest and requires standardization of curricula to meet the best available standards.
- Collaborative work between all stakeholders to optimize pharmacy practice.
- Develop clear accreditation, registration, and classification standards and processes.
The pharmacy profession in the Middle East is evolving, Further development and optimization are obviously anticipated, and pharmaceutical services are expected to improve dramatically in the near future.
Here is an important example of the Clinical Case Presentation
1) HPI (History of Present Illness)
Example:
R.F., a 54-year-old man, presents to the emergency room with a 2-day history of left lower extremity edema, redness, and pain that limits his normal daily activities. The lesion is not elevated and has poorly defined margins.
2) PMH: Past (or Prior) Medical History
Example:
Hypertension (HTN), dyslipidemia, and depression.
3) Medications: What are the Medications the Patient take?
4) SH (Social History): What about Social History?
5) FH (Family History): What about Family History?
6) ROS (Review of Systems): Clinically, many women require drug treatment during pregnancy due to chronic conditions such as epilepsy, diabetes, hypertension, or asthma.
7) PE (Physical Examination)
8) Lab:(2 months prior to presentation) or (past Lab Results if present):
- Risk Summary, Clinical Considerations, Data
- The Lactation subsection
It provides information about using the drug while breastfeeding, such as the amount of drug in breast milk and potential effects on the breastfed infant.
- The Females and Males of Reproductive Potential subsection (8.3):
New to the labelling, includes information, when necessary, about the need for pregnancy testing.
Additionally, the contraception recommendations, and information about infertility as it relates to the drug.
Moreover, Pregnancy Testing, Contraception, Infertility
9) Pharmacotherapy Intervention: What is your Pharmacotherapy Intervention?
“Systematic Thinking in Clinical Cases Help to take the right clinical decision”
Vision #4: Patient Counseling and Education
“Every pharmacist Should Learn the Guidelines for Patient Counselling and Education“
Patient counselling is defined as providing disease or medication information orally or in written form to the patients or their representatives on directions of use.
Information can be a piece of advice on side effects, precautions, storage, diet and lifestyle modifications.
The pharmacist should be perceived as a professional who offers pharmaceutical care
Education Vs. Counseling

Key Clinical Concepts:
The order of thinking, making decisions and acting always is patient first, medical condition (diagnosis) second, and medications third.

Steps during patient Counseling
Main Concepts ??
Counselling is a two-way communication process and interaction between patient and pharmacist, for counseling to be effective.
- Preparing for the session.
- Opening the session.
The patient should be counseled in a semi-private, or private area.
Topics commonly covered include??
- Name and strength of the medication.
- The reason why it has been prescribed or how it works
- How to take the medication
- Expected duration of treatment, benefits of treatment.
- Possible SE, medication or dietary interaction.
- Advice on correct storage.
- Minimum time duration to show therapeutic benefit.
- What to do if a dose is missed.
- Special monitoring requirements, e.g blood tests.
Important Resources for Patient Counseling and Education
Patient Counseling and Education resources provide important Teaching and practising resources for patients and families with important information about medications counseling.
They offer a number of services for patient education and counseling that patients can understand it clearly.
1- PEC: Patient Education and Counseling
The Leading International Journal for Communication in Healthcare
Patient Education and Counseling is published by Elsevier, It is the official journal of the European Association for Communication in Healthcare (EACH) and the American Academy on Communication in Healthcare (AACH).
2- Pharmaceutical Care Practice:
The Patient-Centered Approach to Medication Management Services, 3e Robert J. Cipolle, Linda M. Strand, Peter C. Morley
This book is written for health care practitioners and those involved in the many aspects of our health care systems.
The purpose of the book is to provide the basic information necessary to establish, support, deliver and maintain medication management services.
Additionally, it helps to achieve the goals of therapy essential to the highest level of optimal clinical outcomes, and directly contribute to improving the patient’s quality of life.
Patients deserve no less!
Robert J. Cipolle, PharmD
Linda M. Strand, PharmD, PhD, DSc (Hon)
Peter C. Morley, PhD
3- Lexicomp – Clinical Drug Information
Helps healthcare professionals by providing the most trusted drug and clinical information available, delivered across multiple platforms, and easily integrated.
A hospital-wide solution for pharmacists, physicians and nurses, Lexicomp Online provides clinicians access to two drug information resources within a single interface.
Lexicomp – provides clear, concise, point-of-care drug information, including dosing, administration, warnings.
It also provides an important resource for patient education translated into many languages.
4- ASHP Guidelines on Pharmacist-Conducted Patient Education and Counseling
The Goal of Patient Counseling and Education
Trusting Relation

Part 1: What About Patient Counseling? & Evaluate a Patient Case or Prescription
Part 2: Disease Counseling & Medication Counseling
Part 3: Results, and Recommendations for the Patient
Part 4: Verify the patient understanding for all counseling notes
Patient Counseling and Education is Important to convert the scientific Information into Plain, Easily understood Language
“Joining FADIC Patient Counseling and Education program will help you to know all the guidelines of patient counseling.
Also, FADIC Patient Counseling program provides important counseling information in different medical specialities, such as CVS, CNS, Endocrine, GIT, Obstetrics, and others”
Vision #6: Medication Therapy Management
Bundles of MTM are Pharmacist medication reviews, Health education, Health counseling using motivational interviewing, and Follow up calls at scheduled intervals
Medication Therapy Management “MTM”
- MTM focuses on ongoing management of the patient’s entire medication regimen with a concentration on optimizing therapeutic effectiveness, preventing adverse events.
- Active involvement of patients is critical, empowering them to be a full participant in their own care through better understanding and use of their medications.
What is Medication Therapy Management (MTM)?
- A range of services provided to individual patients to optimize therapeutic outcomes. (help patients get the most benefit from their medications)
- Then, detect and prevent costly medication problem.
MTM provided by pharmacists, the medication therapy expert, results in:
- A review of all medications prescribed by all prescribers providing care to the patient, and any over-the-counter and herbal products the patient may be taking to identify and address medication problems.
- Problems may include medications not being used correctly, duplication of medications, unnecessary medications, and the need for medication(s) for an untreated or inappropriately managed condition.
- In-depth, medication-related education, consultation, and advice provided to patients, family and/or caregivers to help assure proper use of medications.
- Collaboration with the patient, physician, and other health care providers to develop and achieve optimal goals of medication therapy.
Approaches to MTM services-Models
- The key principles of motivational interviewing are the expression of empathy, acceptance of resistance to behaviour change, resolving discrepancies between the provider’s point of view and the patient’s point of view, and supporting self-efficacy.
Santhi Masilamani
Practical Case Scenarios in MTM
Uncontrolled Asthma
- CM, 37, suffers from uncontrolled asthma, unresponsive depression, pain and nausea. She sees multiple specialists, takes many medications (19) and is an expensive patient in her demographic group.
Before MTM:
- CM spent about $2,900 a year on her 19 medications
MTM review:
- CM pharmacists identified five clear problems. Clara overused her short-acting inhaler and lacked a prescription for a long-acting controller inhaler. In addition, one of her 19 medications was a duplicate therapy. In addition, Clara wasn’t taking any medication for depression.
After MTM:
- CM dropped the duplicate therapy and was referred to a physician to restart depression treatment. She stopped using a rescue inhaler as maintenance medicine and got a long-term controller.
Savings:
- MTM repositioned Clara to avoid emergency rooms and hospital admissions, events that would have cost an estimated $24,500. Clara’s two new medications – for depression and long-term asthma control – added just $188 a year to her total medication bill. Total net savings: $21,419.
MTM Economics:
- Asthma patients who use MTM are six times less likely to have an ER/hospital event, according to The Asheville Project’s
Keeping patients out of the hospital is one of the most important and most cost-effective goals of the patient- centred medical home (PCMH)
Vision #7: Comprehensive Medication Management “CMM”
What is CMM?
- CMM is defined as the standard of care that ensures each patient’s medications:
(i.e., prescription, non-prescription, alternative, traditional, vitamins, or nutritional supplements)
- The individually assessed to determine that each medication is appropriate for the patient, effective for the medical condition, safe given the comorbidities and other medications being taken, and able to be taken by the patient as intended.
- CMM includes an individualized care plan that achieves the intended goals of therapy with appropriate follow-up to determine actual patient outcomes.
- This all occurs because the patient understands, agrees with, and actively participates in the treatment regimen, thus optimizing each patient’s medication experience and clinical outcomes.
How is CMM delivered?
- Clinical pharmacists work in collaboration with other providers to deliver CMM that optimizes patient outcomes.
- Care is coordinated among providers and across systems of care as patients transition in and out of various settings.
- The clinical pharmacist’s process of care comprises the following components.
What is the value of CMM?
- The value of CMM is realized in multiple ways by multiple groups.
- Most importantly, patients benefit from improved medication-related clinical outcomes.
- Patients also benefit directly from the increased individualized attention to medications and their impact on their daily lives.
- Physicians and other care team members benefit when clinical pharmacists apply their pharmacotherapeutic expertise in a collaborative process to help manage complex drug therapies.
- Physicians can dedicate more time to the diagnostic and treatment selection process, enabling them to be more efficient, see more patients, and spend more time providing medical care.
- Assessment of the Patient
- Review medical record using a problem-oriented framework (e.g. subjective and objective information) to determine the clinical status of the patient
- Obtain and document complete medication history
- Obtain, organize, and interpret patient data
- Prioritize patient problems and medication-related needs
- Evaluation of Medication Therapy
- Assess the appropriateness of current medications (health conditions, indication, and the therapeutic goals of each medication)
- Evaluate effectiveness, safety, and affordability of therapies
- Assess medication-use and adherence of therapies
- Identify medication-related problems and evaluate collaboratively the need for intervention(s)
- Development & Initiation of Plan
- Review the patient’s active medical problem list for individualized assessment and plan for optimizing therapies
- Formulate a comprehensive medication management assessment and plan to achieve patient-specific outcomes
- Educate patient/caregivers to ensure understanding of the plan, optimize adherence, and improve therapeutic outcomes
- Establish patient-specific measurable parameters and time frames for monitoring and follow-up
- Follow-up & Medication Monitoring
- Coordinate with other providers to ensure that patient follow-up and future encounters are aligned with the patient’s medical and medication-related needs
- Revisit medical record to obtain updates on the clinical status medication-related needs
- Conduct ongoing assessments and refine care plan to optimize medication therapy and ensure that individual goals are achieved
- Monitor, modify, document, and manage the care plan
Vision #8: Medication Management & Use
Essential Safety Requirements in Medication Management & Use is a Must for all Pharmacists
- Medication safety is a fundamental responsibility of all members of the profession of pharmacy
- The medication safety leader’s role includes responsibility for leadership, medication safety expertise, influencing practice
change, research, and education.
The Pharmacist Roles In Medication Safety
- Pharmacists are uniquely qualified to
fill the roles and meet the responsibilities of the medication
safety leader in hospitals and health systems.
Medication Safety
- The landmark Institute of Medicine (IOM) report To Err Is Human: Building a Safer Health System generated major patient safety initiatives.
- Created by government agencies, regulatory and accrediting bodies, professional and organizational associations, and health care organizations.
- The Joint Commission National Patient Safety Goals (NPSGs) are an example of a response to the original IOM report.
- The Pharmacy Practice Model Initiative 4 and the National Quality Forum Safe Practice 185 incorporate medication safety principles to ensure optimal patient safety and outcomes.
Essential Safety Requirements in Medication Management Use “ESR“

- High-Alert Medications “HAM”
Medications that bear a heightened risk of causing significant patient harm when used in error.
Ex.: Concentrated Electrolytes
- Concentrated Magnesium Sulfate 50%.
- Hypertonic Saline (Concentration of more than 0.9% Solutions).
- The undiluted injectable solution of potassium chloride, potassium phosphate, and potassium acetate.
A mandatory Independent double-checks shall be conducted by two nurses prior to administration to include all elements of a correct order:
1) Right Patient “2 Identifiers”
2) Right Drug
3) Right Dose
4) Right Frequency
5) Right Route of Administration.
6) Right Time of Administration.
7) Right Documentation.
The double check will be documented in the medication administration sheet.
All patient receiving high alert medications must be closely observed and monitored.
Separated in the storage areas, Tallman lettering labels, Auxiliary precautionary labels.
1- Hazardous Medications and Chemicals
- A hazardous drug: Drug which poses a significant risk to a healthcare worker by virtue of its teratogenic, mutagenic, carcinogenic, or reproductive toxicity potentials, as well as acute or chronic toxicity to an organ or system.
- MSDS (Material Safety Data Sheet) A form containing data regarding the hazardous properties of chemicals and other hazardous agents.
- The hospital should have a plan for the safe use of these medications.
- Additionally, develop the annually updated list of these medications and Hazardous pharmaceutical chemicals. Handlings of Hazardous Drug Policy by Spill Kits, and MSDS.
2- Look-Alike, Sound-Alike Medications “LASA”
These refer to names of drugs/medications which, due to their pronunciation, may sound similar to other drugs/medications’ names.
In addition, the distribution/administration of these medications may be prone to errors.
This refers to names/shape and package of drugs which, due to their spelling, and or colouring may look similar to other drugs/medications’.
The prescribing dispensing and administration of these medications is subject to errors.
They are common, account for 25% – 30% of Medication Errors, the potential for serious error due to confusing medication names is significant.
Action Plan:
1- Identify your LASA list.
2- Post inpatient care units.
3- Write a complete drug order.
4- Use both generic and brand name.
5- Write an indication or diagnosis:
Omeprazole “Losec” 40 mg tablet PO daily “Peptic Ulcer”
Furosemide “Lasix” 40 mg tablet PO daily “Diuresis”
6- Minimize verbal and telephone orders. Never allowing for Narcotics, Chemotherapeutics, ….. etc.
7- Alert your patient, during counseling, to avoid mixing up LASA medications.
8- Encourage patients to question nurses about medications that are unfamiliar or look or sound different than expected.
9- Separate LASA medication on the shelf.
10- Affix name “Alert” on LASA medications.
11- Use boldface, or Tall man letter, the parts of names that are different “Computerized Prescriber Order Entry”
gliPIZide – gliclazide
gliMEPIRide – gliBENCLAMide
12- Independent double check in dispensing, and administrating processes should be applied.
13- Report any errors and potentially hazardous conditions with LASA product names to help develop strategies to reduce them.
14- Avoid purchase of LASA medications.
3- Medication Errors and Near Miss
In 1999 landmark paper:
- “To Err is Human” the US Institute of Medicine stresses to face the medical errors, that was the eighth cause of death in the US.
- Every hospital is probably subjected to at least one medication error every day.
Is any PREVENTABLE event that may cause or lead to inappropriate medication use or potential harm while the medication is in the control of healthcare professionals, patient, or consumer.
Near-Miss:
An event that could have resulted in unwanted consequences, but didn’t because either by chance or through timely intervention the event didn’t reach the patient.
At-Risk Behavior
Chance of ignoring an established safety policy or
procedure.
Examples:
- Not wearing gloves.
- Not following established safety procedure.
Shortcuts
- What is easiest isn’t always what is safest !!
4- Medication Errors Reporting Process
- Error identification
- Assess Patients
- Inform the Nurse, pharmacy, physician “timeframe”
- Medication safety officer “MSO” clinical investigation.
- Quality department feedback report with MSO.
- Feedback report received by the corresponding nurse.
- Discuss error in P&T Committee.
- Errors that harm the patients reported in MR.
Basics of Medication Safety
DOUBLE CHECK!!
Get information on how to take the medication… THEN….Tell your pharmacist your understanding of how to take the medication
Report and Learn from Medication Incidents

- Inform healthcare providers if you feel a medication incident has occurred
- Reporting incidents help get to the root of the problem
Reporting Adverse Drug Reactions
- Adverse drug reactions are not related to the healthcare provider
- Report adverse drug reactions to the Vigilance Program.
Vision #9: Effective Communication
Pharmacist Intervention is important to maintain effective communication with the prescriber physicians
The trained and qualified pharmacist shall review the order for:
- Patient’s allergies or sensitivities.
- Approved indications for use.
- Therapeutic duplications.
- Existing or potential interactions: Such as the drug-drug, and the drug-food interaction.
- Appropriateness of the medication: As dose, frequency, route of administration, Contraindications.
Vision #10: TPN, IV admixture
Giving a patient a contaminated product can cause serious adverse effects including death. So, the safety of intravenous admixture product depends on the skills, compliance with aseptic techniques, and IV room cleanliness.
IV Admixture
- Parenteral medications account for > 40% of all medications administered in institutional practice.
- The intravenous route is the most dangerous route of administration since all natural barriers are bypassed when the drug is given directly into the vein, so the administration of contaminated solution can have very serious consequences.
- It is essential to control all these different sources at the time the aseptic technique is carried out.
IV Room Cleanliness
- Giving a patient a contaminated product can cause serious adverse effects including death.
- The safety of intravenous admixture product depends on the skills of the operator, compliance with aseptic techniques, and IV room cleanliness.
Clean Room & LAFH
- Clean room design, equipment and cleanliness are pre-requisite for aseptic technique.
- Proper selection and maintenance of equipment prevent any break-through aseptic procedure.
- The pharmacy regularly monitors the performance of laminar airflow hood (LAFH) and maintains updated certification.
- Chemotherapy admixture area is completely separated from regular IV area
Clean Room Design
ISO Classification
ISO Classification of Particulate Matter in Room Air (limits are in particles of 0.5 µm and larger per cubic meter [current ISO] and cubic feet.
For example, 3,520 particles of 0.5 micron per m3 or larger (ISO Class 5) is equivalent to 100 particles per ft3 (Class 100) (1 m3 = 35.2 ft3).
Pressure Differential Monitoring
- Between buffer area and ante-area
- Between ante-area and the general environment outside the compounding area.
- The frequency of monitoring: at least daily (ideally every shift).
- The pressure between ISO 8 and general environment should not be less than 5 Pascal (0.02-inch water column).
ISO Class 5 Air Sources
- LAFHs are the most common sources of ISO Class 5 air quality for exposure of critical sites.
- Laminar Air Flow Hood (LAFH): Is a device used for high – efficiency particulate air (HEPA) filtration which provides sterile environments for the preparation of IV and other sterile products.
- HEPA filter: High-efficiency particulate air filters, which remove 99.97% of all particles 0.3 microns or larger.
Buffer Areas
- A clean room is a compounding environment that is supplied with HEPA or HEPA-filtered air that meets ISO Class 7.
- This is to access to it is limited to personnel trained and authorized to perform sterile compounding and facility cleaning.
Ante-area
- An ISO Class 8 or better area where:
- Personnel hand hygiene and garbing procedures (aseptic technique starts in this area)
- Staging of components,
- Order entry,
- CSP labelling,
- High particulate generating activities are performed.
- Transition area that provides assurance that pressure relationships are constantly maintained so that air flows from clean to dirty area.
Ante-Room
- In this area, the aseptic technique should be started.
- It should contain; sink, soap dispenser, stainless steel shelves to store disposable materials required for aseptic technique, e.g. Gloves, gowns, mask, shoe cover, etc.
Facility Design and Environmental Controls
- Minimizes air born contamination
- Comfortable (temperature ≤ 20 ⁰C)
- Well-lighted working environment
- ISO Class 7 buffer area and ante-area supplied with HEPA-filtered air.
- Equipment
- Furniture
- Supplies
- Head Cover
- Shoe Cover
- Masks and Gloves
Personnel Garbing
- Hairnet
- Beard cover
- Face mask
- Gown
- Gloves
- Shoe covers
Compounding Sterile Preparations
- Mops floors, using the mop labelled “floors”, separated for the clean room
TPN Formulation
- Parenteral nutrition formulations are extremely complex admixtures containing:
- amino acids,
- dextrose,
- fat emulsions,
- water,
- electrolytes,
- trace elements,
- multivitamins,
- Serious harm and death have been reported secondary to administration of improperly prepared, and/or contaminated parenteral nutrition formulations.
Annual Evaluation of service provided by contract
- Annual Evaluation of service provided by contract
TPN Compounding
- Many hazardous drugs such as the compounding of these products is regulated by the United States Pharmacopeia (USP), chapter 800.
- Must ensure the safety of personnel involved according to OSHA guidelines and protect patients from improperly compounded sterile preparations by regulating facilities.
- Moreover, equipment, and work practices to ensure the sterility of extemporaneously compounded sterile preparations.
Shoe Covers & Masks
- Remove shoe covers with a gloved hand before leaving area Discard shoe covers as hazardous waste
- Surgical masks DO NOT provide adequate protection Use a NIOSH approved respirator (N95)
Vision #11
Handling Hazardous Chemotherapy
Spill Control
- Use of PPE’s (including respirators)
- Spill kit (readily accessible)
- Eyewash station and shower station
- MSDS (readily accessible)
Vision #12: Extemporaneous Preparations
Ensure all structural requirements are available and enough (sink, alcohol dispensers, antiseptic soap, cleaning tools)
Compounding Non-Sterile Preparations
The hospital has a system for safe preparation of non-sterile compounded preparations (extemporaneous compounds).
Proper Compounding Area
- The compounding area should be located sufficiently away from routine dispensing.
- Proper temperature and humidity control within the compounding area or facility is desirable.
- Eye Wash station and spill kits
Proper Equipment
Measuring: Balance, weights, weighing containers, volumetric glassware (graduates, pipets, flasks, syringes).
Mixing: Beakers, flasks, spatulas, funnels, sieves, mortar and pestle
Packaging: bottles, ointment jars.
Preparation Manual & MSDS
-
- Pharmacists and Supportive personnel must have ready access to reference materials on all aspects of compounding

Preparations Log Book
- The pharmacist shall record the name of the prepared medicine, strength, prepared quantity, batch number, expiration date, and the preparation number on the log book.
Important Tips
Use appropriate final containers:
- Final containers and closures should be clean and free from dust and other residues. Light protective (e.g. dark
- plastic or amber glass) containers should generally be used.
Expiry dates: (BUD)
- It is recommended that an expiry date of a maximum of one month (or less if advised in the published study) is applied to all extemporaneous formulations.
Pharmacy Infection Prevention and Control
- The pharmaceutical care enforces the hospital guidelines for infection prevention and control.
Hand Washing
- As the hands of health-care workers are the most frequent vehicle of nosocomial infections, hand hygiene — including both hand washing and hand disinfection — is the primary preventive measure.
Following Hospital Standard Precautions
Proper Cleaning of Laminar Flow Hood
- Use isopropyl alcohol 70% to disinfect the compounding area prior to the beginning of each shift
- Allow alcohol to dry (dryness time is the bacterial killing time).
- Clean from back to front and top to bottom and avoid contact and contamination of the HEPA filter
Action Plan
- Participate in Infection control committee
- Attend training
- Conduct observational audits
- Post educational and reminder signs
- Communicate policies and procedures
Vision #13
Learn How to apply an EBM into your clinical practice
Evidence-Based Practice learning Series: The 5A’s Steps of EBM
Why?
- You may not have enough Time
- You may not have effective skills
- You may not have the proper resource
- The Question is: WHERE is the most useful information?
Resources and Hierarchy of Evidence(s)
– The checklists have been developed to help this process to be easy; however, they all focus in three areas:
- Validity.
- Results.
– Critical Appraisal skills help health providers decision makers develop skills in assessing evidence about clinical effectiveness.

There are three basic questions that need to be answered for every type of study:
- Are the results of the study valid?
- It examines the methodology of the study.
- It is called “Internal Validity”.
- Are the results of the study important?
- The magnitude of the results and its significance.
- It examines the Results of the study.
- Will the results help in caring for your patient?
- Applicability of these results to his/her patients.
- It is called “External Validity”
Specific Appraising Guide for each Type of Study
You can find the appraising guides for the different types of articles by clicking on the links below:
- Worksheet for using an article about therapy or prevention.
- Worksheet for using an article about Diagnosis.
- Worksheet for using an article about Prognosis.
- Worksheet for using an article about Systematic Review.
Barriers and Overcome Strategy: Barriers and Overcome Strategy to apply the evidence to patients

Assess !!
- Assessing the whole Evidence-Based Practice
- Outcome assessment and re-evaluation of the process are integral parts of the EBP concept.
- It can help Healthcare identify gaps in skills and research.
- The more EBP is used, the more challenges and the more experience gained.
Approach for Assessing the EBP Cycle
The Center for Evidence-Based Medicine Toronto suggested some approaches for doing this in the lists that follow:
Assessing in Asking Answerable Questions
- Am I asking any clinical questions at all?
- Am I asking well-formulated (PICO) questions?
- Am I using a “map” to locate my knowledge gaps?
- Can I get myself unstuck when asking questions?
- Do I have the method to save questions for later answering?
- Is my success rate of asking answerable questions rising?
Assessing in Finding the Best Evidence
- Do I know the best sources of current evidence?
- Have I achieved access to searching hardware, software?
- Am I finding useful evidence from a widening of sources?
- Am I becoming more efficient in my searching?
- Am I using MeSH headings, limiters, and intelligent, free text when searching MEDLINE?
Assessing in Critically Appraising the Evidence for Validity and Usefulness
- Am I critically appraising external evidence at all?
- Are critical appraisal guides easier for me to apply?
- Am I becoming more accurate and efficient in applying some of the critical appraisal measures (such as likelihood ratios, and NNTs)?
Assessing in Integrating the Critical Appraisal with Clinical Expertise and Applying the Result in Clinical Practice
- Am I integrating my critical appraisals into my practical?
- Am I becoming more accurate and efficient in adjusting critical appraisal measures to fit my patients?
- Can I explain disagreements about management decisions in terms of this integration?
- Have I conducted any clinical decision analyses?
EBM Integration
Evidence-Based Medicine (EBM) is the integration of clinical expertise, patient values, and the best research evidence into the decision making the process for patient care.
Vision #14
What about Clinical Research?
Clinical research is the study of health and illness in people. It is the way we learn how to prevent, diagnose and treat illness.

Vision #15:
Implementation of the Antimicrobial Stewardship Systematic Thinking Approach in any Infectious Disease Clinical Case
Learn how to apply the Antimicrobial Stewardship Program will learn you the Systematic Way in thinking in Infectious Disease Cases.
In addition to Implement Stewardship into your Organization
Vision #16
Leadership in clinical practice and Lifelong Learning Develop a personal plan for implementing the Model for Lifelong learning activity for education
Why ??
Why is it important to develop a culture of lifelong learning across the curriculum?
Importance of teaching life‐long learning habits
Ask yourself:
- How relevant is the information I was taught in pharmacy college?
- How do YOU make sense of new information?
- How should new information be compared and contrasted with older information?
- Has the standard of care remained the same? Has it changed?
- Why has it changed?
- Has new safety information emerged? Has new evidence emerged? Is it compelling?
- How do YOU keep up with new information?
The Balance of Keeping Up: Knowledge, skills, values and abilities Opportunities for Self‐directed Lifelong Learning
Limitations:
- We cannot teach everything!
- Time constraints
- Efficiency in how information is obtained
- Content/resources provided vs. independently
- New information changes daily
- New medications
- Newly published guidelines

Education Quotes !!
Education is not the learning of facts, it’s rather the training of the mind to think.
I never teach my pupils; I only attempt to provide the conditions in which they can learn.
Albert Einstein
When do you have to “enhance” coursework?

Education Quotes !!
Education isn‘t something you can finish
Example of Literature Activity Designing the Activities
Model lifelong learning
- Compare and contrast answers to structured self‐assessment questions
- Discussion of journal club
- Examine whether the evidence will change how we manage patients?
- Solve “paper” patient cases
- Application of information in actual patient care situations
Reflection on Example Literature Activity
Advantages:
- Opportunity to model lifelong learning
- Shared workload
- Adaptable across practice settings
- Flexibility in scheduling activities
- Allows for periodic updating
Disadvantages:
- Initially labour intensive
- Variability in practice settings
- Variability in the rotation sequence
Professional Education
- Prioritize the needed & required learning topics.
- Weekly Improvement Topics.
- Monthly Improvement Curriculum.
- Training, Competency, and Certification.
What about Interprofessional Education?
![]()
Vision #17
Know the 7 Habits of Highly Effective People
The 7 Habits for Highly Effective Pharmacists?

Vision #18
Know the 7 Habits for Highly Effective Pharmacists, and be effective
Leadership ??
- Lead your life, Lead yourself
- Learn how to be a great Pharmacist “From Good to Great”
- Put the Mission for your life
- Learn how to lead others
- How to put the strategic plan for yourself, and for the organization.
Vision #19
Learn How to be an Effective Leader for yourself and others
“We have resources—which include personal time, energy, talent, and wealth—and we are using them to try to grow several “businesses” in our personal lives. These include having a rewarding relationship; raising great children; and succeeding in our careers.
Recommended Readings:
1- “How Will You Measure Your Life?

2- 7 Habits of Highly Effective People
3- Good to Great: Why Some Companies Make the Leap…And Others Don’t Kindle Edition
What about YOU !!!
NOW, Create your Vision ..
FADIC Certificates
If you Don’t have time to Read, You can Download the Whole 2030 Vision from Here. Kindly Enter your Email to Download the Whole 2030 Vision!!

Read More:
- Drug Information Program and Workshop
- Evidence-Based Program
- Patient Counseling and Education
- Roadmap to Antimicrobial Stewardship Program
- Pharmacist Guide Program
- Biostatistics Clinical Guide
- FADIC Blog in English
- Arabic FADIC Blog
- FADIC Programs and Courses
- Download Now the Info-graphic of Patient Centered-Care, from this LINK.

 Log in
Log in Sign up
Sign up