Haemoglobin
Haemoglobin
Anaemia is defined as a low number of red blood cells. This is all about Haemoglobin
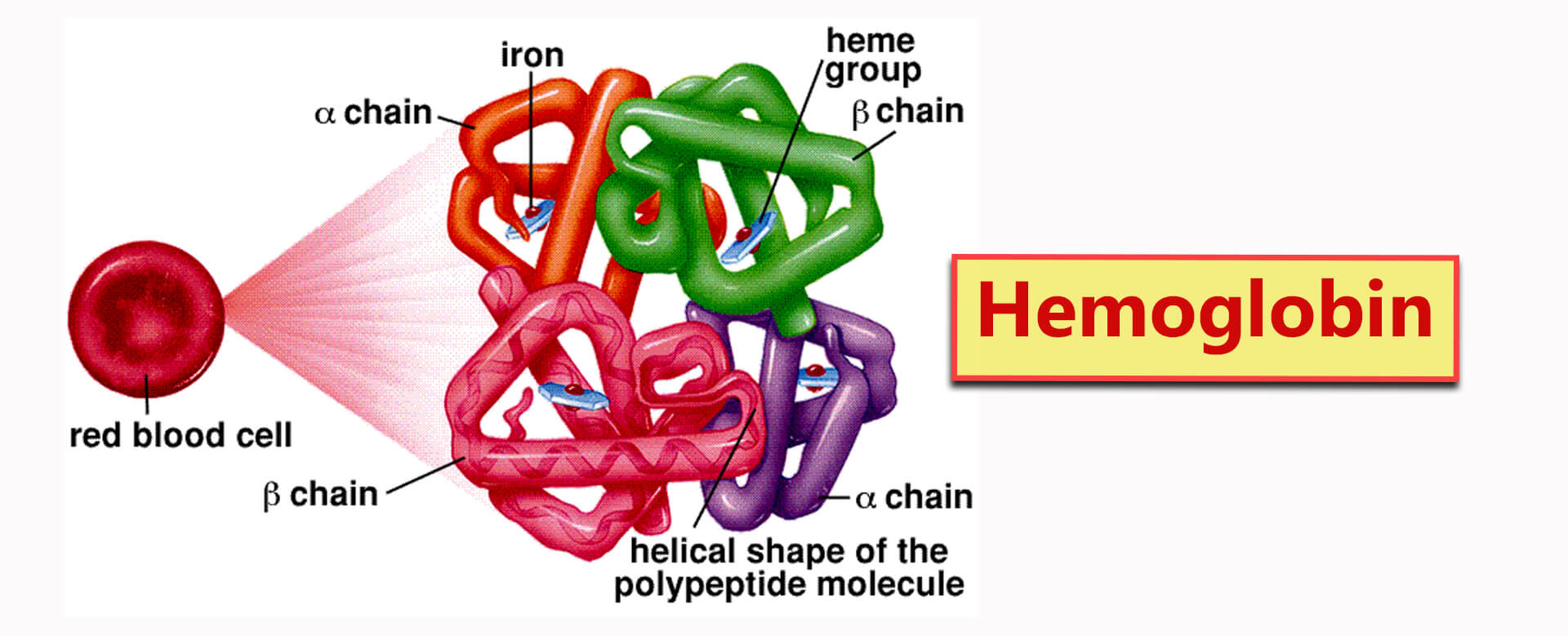
A routine blood test reports anaemia as low haemoglobin or hematocrit. Haemoglobin is the main protein in your red blood cells.
It carries oxygen and delivers it throughout your body.
If you have anaemia, your haemoglobin level will be low too. If it is low enough, your tissues or organs may not get enough oxygen.
Symptoms of anaemia — like fatigue or shortness of breath — happen because your organs aren’t getting what they need to work the way they should.
Anaemia is the most common blood condition in the U.S. It affects almost 6% of the population. Women, young children, and people with long-term diseases are more likely to have anaemia. Important things to remember are:
- Specific forms of anaemia are passed down through your genes, and infants may have it from birth.
- Women are at risk of iron deficiency anaemia because of blood loss from their periods and higher blood supply demands during pregnancy.
- Older adults have a greater risk of anaemia because they are more likely to have kidney disease or other chronic medical conditions.
There are many types of anaemia. All have different causes and treatments. Some forms — like the mild anaemia that happens during pregnancy — aren’t a major concern. But some types of anaemia may reflect a serious underlying medical condition.
Anemia Symptoms
The signs of anaemia can be so mild that you might not even notice them. As your blood cells decrease, symptoms often develop at a certain point. Depending on the cause of the anaemia, symptoms may include:
- Dizziness, lightheadedness, or feeling like you are about to pass out
- Fast or unusual heartbeat
- Headache
- Pain, including in your bones, chest, belly, and joints
- Problems with growth for children and teens
- Shortness of breath
- Skin that’s pale or yellow
- Cold hands and feet
- Tiredness or weakness
Anaemia Types and Causes
There are more than 400 types of anaemia, and they’re divided into three groups:
- Anaemia is caused by blood loss
- Anaemia is caused by decreased or faulty red blood cell production
- The destruction of red blood cells causes anaemia
Anemia Caused by Blood Loss
You can lose red blood cells through bleeding. This can happen slowly over a long period of time, and you might not notice. Causes can include:
- Gastrointestinal conditions such as ulcers, haemorrhoids, gastritis (inflammation of your stomach), and cancer
- Non-steroidal anti-inflammatory drugs (NSAIDs) such as aspirin or ibuprofen can cause ulcers and gastritis
- A woman’s period, especially if you have heavy menstruation (or heavy period). This can be associated with fibroids.
- Post-trauma or post-surgery as well.
Anemia Caused by Decreased or Faulty Red Blood Cell Production
With this type of anaemia, your body may not create enough blood cells, or they may not work the way they should.
This can happen because there’s something wrong with your red blood cells or because you don’t have enough minerals and vitamins for your red blood cells to form normally. Conditions associated with these causes of anaemia include:
- Bone marrow and stem cell problems
- Iron-deficiency anaemia
- Sickle cell anaemia
- Vitamin-deficiency anaemia, specifically b12 or folate
Bone marrow and stem cell problems
may keep your body from producing enough red blood cells. Some of the stem cells in the marrow that’s in the centre of your bones will develop into red blood cells. If there aren’t enough stem cells, if they don’t work right, or if they’re replaced by other cells such as cancer cells, you might get anaemia. Anaemia caused by bone marrow or stem cell problems includes:
- Aplastic anaemia happens when you don’t have enough stem cells or none. You might get aplastic anaemia because of your genes or because your bone marrow was injured by medications, radiation, chemotherapy, or infection. Other malignancies that commonly affect the bone marrow include multiple myeloma or leukaemia. Sometimes, there’s no clear cause of aplastic anaemia.
- Lead poisoning. Lead is toxic to your bone marrow, causing you to have fewer red blood cells. Lead poisoning can happen when adults come into contact with lead at work, for example, or if children eat lead paint chips. You can also get it if your food comes into contact with some types of pottery that aren’t glazed right.
- Thalassemia has a problem with haemoglobin formation (4 chains aren’t correctly formed). You make really small red blood, cells-though you can make enough of them to be asymptomatic, or it can be severe. It’s passed down in your genes and usually affects people of Mediterranean, African, Middle Eastern, and Southeast Asian descent. This condition can range from mild to life-threatening; Cooley’s anaemia is the most severe form.
Iron-deficiency anaemia
It happens because you don’t have enough of the mineral iron in your body. Your bone marrow needs iron to make haemoglobin, the part of the red blood cell that takes oxygen to your organs. Iron-deficiency anaemia can be caused by:
- A diet without enough iron, especially in infants, children, teens, vegans, and vegetarians
- Certain drugs, foods, and caffeinated drinks
- Digestive conditions such as Crohn’s disease or if you’ve had part of your stomach or small intestine removed
- Donating blood often
- Endurance training
- Pregnancy and breastfeeding use up iron in your body
- Your period
- A common cause is chronic slow bleed, usually from a Gastrointestinal source.
Sickle cell anaemia
- is a disorder that, in the U.S., affects mainly African Americans and Hispanic Americans.
- Your red blood cells, which are usually round, become crescent-shaped because of a problem in your genes. Anaemia results when the red blood cells break down quickly, so oxygen doesn’t get to your organs. The crescent-shaped red blood cells can also get stuck in tiny blood vessels and cause pain. This is all about Haemoglobin
Vitamin-deficiency anaemia
- can happen when you aren’t getting enough vitamin B12 and folate. You need these two vitamins to make red blood cells. This kind of anaemia can be caused by:
- Dietary deficiency: If you eat little or no meat, you might not get enough vitamin B12. If you overcook vegetables or don’t eat enough of them, you might not get enough folate.
- Megaloblastic anaemia: When you don’t get enough vitamin B12, folate, or both
- Pernicious anaemia: When your body doesn’t absorb enough vitamin B12
Other causes of vitamin deficiency include medications, alcohol abuse, and intestinal diseases such as tropical sprue.
Anaemia is associated with other chronic conditions
usually occurs in the setting of long-standing inflammation. Inflammatory proteins slow the bone marrow’s production of young red blood cells in various ways. Conditions that cause this type of anaemia include:
- Advanced kidney disease
- Hypothyroidism
- Old age
- Long-term diseases include cancer, infection, lupus, diabetes, and rheumatoid arthritis.
Anemia Caused by Destruction of Red Blood Cells
When red blood cells are fragile and can’t handle the stress of travelling through your body, they may burst, causing haemolytic anaemia. You might have this condition at birth, or it could come later. Sometimes, the causes of haemolytic anaemia are unclear, but they can include:
- An attack by your immune system, as with lupus. This can happen to anyone, even a baby still in the womb or a newborn. That’s called haemolytic disease of the newborn.
- Conditions that can be passed down through your genes, such as sickle cell anaemia, thalassemia, and thrombotic thrombocytopenic purpura (TTP)
- Enlarged spleen. This can, in rare cases, trap red blood cells and destroy them too early.
- Something that puts strain on your body, such as infections, drugs, snake or spider venom, or certain foods
- Toxins from advanced liver or kidney disease
- Vascular grafts, prosthetic heart valves, tumours, severe burns, being around certain chemicals, severe hypertension, and clotting disorders
Anemia Diagnosis
A complete blood count (CBC) test will measure your red blood cells, haemoglobin, and other parts of your blood. Your doctor will ask about your family and medical history after the CBC. They’ll probably do some tests, including:
- Blood smear or differential to count your white blood cells, check the shape of your red blood cells and look for unusual cells
- Reticulocyte count to check for immature red blood cells
Anemia Treatment
Your treatment will depend on your type of anaemia. There are a lot of causes, so there are also many treatments available.
- If you have aplastic anaemia, you might need medication, blood transfusions (in which you get blood from another person), or a bone marrow transplant (in which you get a donor’s stem cells).
- If you have haemolytic anaemia, you might need medication that will hold back your immune system. Your primary care doctor may refer you to a doctor specialising in vascular problems.
- If it’s caused by blood loss, you might have surgery to find and fix the bleeding. If you have iron-deficiency anaemia, you’ll probably need to take iron supplements and change your diet.
- Sickle cell anaemia treatment includes painkillers, folic acid supplements, intermittent antibiotics or oxygen therapy. A drug. Hydroxyurea (Droxia, Hydrea, Siklos) is often prescribed to decrease sickle cell pain crises (a complicated mechanism). The medication is called voxelator (Oxbryta), which can help your red blood cells keep their proper shape. Crizanlizumab-tmca (Adakveo) can keep the blood cells from sticking together and blocking vessels. L-glutamine oral powder (Endari) can cut down on your trips to the hospital for pain and also guard against a condition called acute chest syndrome.
- You will be prescribed supplements if you have a vitamin B12 or folate deficiency.
- Thalassemia doesn’t usually need treatment, but if your case is severe, you might have blood transfusions, a bone marrow transplant, or surgery.
8 Types Of Food That Can Help You Fight Anemia
Most anaemic patients are advised to take 150 to 200 milligrams of iron every day.
Make sure to have these foods to fight anaemia:
1) Fruits and Vegetables
- Curly kale and other varieties
- Collard greens
- Pomegranates
- Swiss chard
- Red and yellow peppers
- Watercress
- Spinach
- Dandelion greens
- Oranges
- Strawberries
- Lemon
- Key lime
- Sweet potatoes
- Beet greens
Dark leafy greens like spinach are a great source of non-heme iron. Vitamin C from citrus fruits helps the stomach to absorb iron. Swiss chard and Collard greens are good sources of both Vitamin C and iron.
2) Nuts and Seeds
- Cashews
- Hemp seeds
- Sunflower seeds
- Pumpkin seeds
- Pistachios
- Pine nuts
- Walnuts
- Peanuts
- Almonds
- Hazelnut
Nuts and seeds are some of the most nutrient-dense foods. One ounce of pistachios can provide 6.1% of a person’s required daily value of iron.
3) Meat and Fish
- Lamb
- Liver
- Oysters
- Salmon
- Perch
- Beef
- Venison
- Shellfish
- Shrimp
- Tuna
- Halibut
- Haddock
- Chicken
Meat and fish have heme iron. Lean cut white meat like chicken is a great source of heme protein. Three ounces of grilled chicken with sides of broccoli, sauteed spinach, and tomatoes can make for a great iron-rich meal for people suffering from anaemia.
4) Eggs
Eggs are known for their proteins, but they also pack a high iron level. Eggs can be paired with whole-grain toast, lightly roasted tomatoes, and quinoa for breakfast, providing a great start to the day.
5) Beans and Pulses
- Chickpeas
- Black-eyed peas
- Black beans
- Lima beans
- Kidney beans
- Soybeans
Lentils are supposed to be a superfood for anaemic patients. Half a cup of lentils has about 3.3 milligrams of iron, which is around 20% of your body’s daily needs. Beans and pulses work for vegetarians and meat-eaters and provide a good amount of iron. This is all about Haemoglobin
6) Blackstrap Molasses
Blackstrap molasses are loaded with iron. They are a total nutritional powerhouse because of calcium, Vitamin B6, selenium, and magnesium. They are perfect for anaemic patients because apart from providing the iron they desperately need, blackstrap molasses also keep them healthy due to the presence of other integral nutrients.
7) Grains
Iron-fortified pasta, cereals, and grains are good options for getting the much-needed iron. However, there are natural options too. They are all rich in iron and can help shoot up the blood’s haemoglobin level.
- Quinoa
- Oats
- Whole wheat
- Kamut
- Teff
8) Fortified Food
Different types of food are fortified with iron. You can add these to your diet if you are a vegetarian or cannot keep down other sources of iron.
- Fortified, ready-to-eat cereals
- Fortified pasta
- Fortified white rice
- Fortified orange juice
- Foods made from fortified white flour, like bread
- Foods made from fortified cornmeal
Foods to Avoid if You Are Anaemic
Some types of food interfere with the absorption of iron. As a result, having all that iron-rich food sometimes might prove to be redundant if had with these foods:
- Yoghurt
- Raw milk
- Cheese
- Sardines
- Broccoli
- Tofu
- Tea and coffee
- Food containing tannins like corn, grapes, sorghum
How Can You Get More Iron From Your Diet?
- Have food rich in iron
- Include food in your diet that will help you absorb the iron
- Cook food in a cast-iron skillet
- Cook food for shorter periods
- Refrain from drinking tea or coffee with meals
- Consult with your doctor and choose supplements containing ferrous salts
How Does Your Body use Iron From Iron-Rich Foods?
- The iron from iron-rich foods is absorbed through the upper part of the small intestine.
- Dietary iron is of two types: heme iron and non-heme iron. Heme iron is derived from haemoglobin.
- Our body absorbs iron mostly from heme sources. Heme iron can be found in fish, red meats, and poultry. Non-heme iron is mainly found in plant sources. Meat, seafood, and chicken contain a little bit of both.
- Following dosage instructions is essential because excess iron can cause iron toxicity. Consult with your doctor, go to a dietician if required, and get a proper diet chart. No one food can cure anaemia, but the right diet can help a lot. Follow it well, and anaemia shouldn’t pose to be a problem anymore.
This is the normal range & how to treat low haemoglobin – Reference Range
The reference ranges for haemoglobin (Hb) concentrations in adults are as follows:
- Male: 14-18 g/dL or 8.7-11.2 mmol/L (SI units)
- Female: 12-16 g/dL or 7.4-9.9 mmol/L (SI units)
- Pregnant female: >11 g/dL
- Elderly: Slight decrease in values
The reference ranges for Hb concentrations in children are as follows:
- New-born: 14-24 g/dL
- 0-2 weeks: 12-20 g/dL
- 2-6 months: 10-17 g/dL
- 6 months-1 year: 9.5-14 g/dL
- 1-6 years: 9.5-14 g/dL
- 6-18 years: 10-15.5 g/dL
Possible critical values:
- < 5.0 g/dL or >20 g/dL
What is low haemoglobin?
- Haemoglobin is a protein in your red blood cells. Your red blood cells carry oxygen throughout your body.
- Oxygen powers your cells and gives you energy. A low haemoglobin level may signify several conditions, including different kinds of anaemia and cancer.
What happens when haemoglobin is low?
- If a disease or condition affects your body’s ability to produce red blood cells, your haemoglobin levels may drop.
- When your haemoglobin level is low, your body isn’t getting enough oxygen, making you feel very tired and weak.
At what level is haemoglobin dangerously low?
- Normal haemoglobin levels are different for men and women.
- For men, a normal level ranges between 14.0 grams per decilitres (gm/dL) and 17.5 gm/dL. For women, a normal level ranges between 12.3 gm/dL and 15.3 gm/dL.
- A severe low haemoglobin level for men is 13.5 gm/dL or lower. For women, a severe low haemoglobin level is 12 gm/dL.
What tests do healthcare providers use to diagnose low haemoglobin?
- Healthcare providers diagnose low haemoglobin by taking samples of your blood and measuring the amount of haemoglobin in it.
- This is a haemoglobin test. They may also analyse different types of haemoglobin in your red blood cells or haemoglobin electrophoresis. This is all about Haemoglobin
What causes haemoglobin levels to go low?
Several factors affect haemoglobin levels:
- Your body doesn’t make enough red blood cells. Your body produces red and white blood cells in your bone marrow.
- Sometimes, conditions and diseases affect your bone marrow’s ability to produce or support enough red blood cells.
- Your body produces enough red blood cells, but the cells are dying faster than your body can replace them.
- You’re losing blood from injury or illness. You lose iron anytime you lose blood. Sometimes, women have low haemoglobin levels when they have their periods.
- You may also lose blood if you have internal bleeding, such as a bleeding ulcer.
- Your body can’t absorb iron, which affects your body’s ability to develop red blood cells.
- You’re not getting enough essential nutrients like iron and vitamins B12 and B9. This is all about Haemoglobin
What affects red blood cell production?
Your bone marrow produces red blood cells. Diseases, conditions, and other factors that affect red blood cell production include:
Lymphoma:
- Lymphoma is a term for cancers in your lymphatic system. If you have lymphoma cells in your bone marrow, those cells can crowd out red blood cells, reducing the number of red blood cells.
Leukaemia:
- Leukaemia is cancer of your blood and bone marrow. Leukaemia cells in your bone marrow can limit the number of red blood cells your bone marrow produces.
Anaemia:
- There are many kinds of anaemias involving low haemoglobin levels.
- For example, if you have aplastic anaemia, the stem cells in your bone marrow don’t create enough blood cells.
- In pernicious anaemia, an autoimmune disorder, keeps your body from absorbing vitamin B12. Without enough B12, your body produces fewer red blood cells.
Multiple myeloma:
- Multiple myeloma causes your body to develop abnormal plasma cells that may displace red blood cells.
Myelodysplastic syndromes:
- This condition happens when your blood stem cells don’t become healthy blood cells.
Chronic kidney disease:
- Your kidneys make a hormone that signals your bone marrow to make red blood cells. Chronic kidney disease affects this process.
Antiretroviral medications:
- These medications treat certain viruses. Sometimes, these medications damage your bone marrow, affecting its ability to make enough red blood cells.
Chemotherapy:
- Chemotherapy may affect bone marrow cells, reducing the number of red blood cells your bone marrow produces.
What affects red blood cell lifespan?
- Your bone marrow constantly produces red blood cells. Red blood cells live about 120 days in your bloodstream.
Some factors that affect that lifespan include:
- Enlarged spleen (splenomegaly).
- Your spleen filters red blood cells as the cells move through your body.
- It traps and destroys damaged or dying red blood cells.
- Some diseases cause your spleen to increase in size.
- When this happens, your spleen traps more red blood cells than usual, essentially ending those cells’ lifespan earlier than usual.
- Sickle cell anaemia. This is a blood disease that affects your haemoglobin.
- Thalassemia. These blood disorders affect your body’s ability to make haemoglobin and red blood cells.
How do you fix low haemoglobin?
- Healthcare providers treat low haemoglobin by diagnosing the underlying cause.
- For example, if your haemoglobin levels are low, your healthcare provider may do tests that reveal you have iron-deficiency anaemia.
- If that’s your situation, they’ll treat your anaemia with supplements.
- They may recommend you try to follow an iron-rich diet. In most cases, treating the underlying cause of anaemia will bring the haemoglobin level up.
What can I do at home to treat low haemoglobin?
- Many things can cause low haemoglobin, and most of the time you can’t manage low haemoglobin on your own.
- But eating a vitamin-rich diet can help maintain your red blood cells.
- A balanced diet focusing on important nutrients is the best way to maintain healthy red blood cells and haemoglobin.
Here are some suggestions:
- Red meat (beef) and meat from the organs, like the liver.
- Leafy vegetables, like kale and spinach.
- Lentils, beans, and peas.
- Nuts and dried berries. This helps in haemoglobin
When should I call my healthcare provider?
- If you have a disease or condition that affects your haemoglobin levels, you should call your healthcare provider anytime your symptoms worsen.
In conclusion:
- If you have blood test results showing your haemoglobin level is lower than normal, you have fewer red blood cells doing essential work — that is, carrying oxygen throughout your body.
- A low haemoglobin level may not be a cause for alarm.
- Many things affect haemoglobin levels. If your test results show low haemoglobin levels, your healthcare provider will explain why you have this symptom, what it means and how it will be treated. This is all about Haemoglobin.
Read More:
- Antimicrobial Stewardship School
- Sepsis Training Program
- Download Pocket Guide for Antibiotic Pharmacotherapy Book
- Microbiology Course | ABC Bacteria
- Infectious Disease E-News | FREE Subscription
- ABC antimicrobials | Know all about the Antimicrobials
- Road Map to Antimicrobial Stewardship Training Program
- Register Now in FADIC Clinical Research School
- FADIC Drug Information Fellowship
- Buy FADIC Toolkit for Writing Research to Write a Great Research Paper
- Read 10 Skills You Must Learn to Do Research via Google Scholar in Arabic
- The FADIC Online Continuous Medical Improvement Programs & Mini-Courses.
- Check Now FADIC Book store and Buy books in different specialities.
- Watch Now FADIC TV to Keep Yourself Updated.
- FADIC Podcast focuses on varieties of pharmacist perspectives in different specialities.
- Subscribe Now to FADIC 2020 Daily News (FNN) and Keep Updated.
- Check Now about Coronavirus Resource Information Center.

 Log in
Log in Sign up
Sign up