Medication Therapy Management in geriatric

Medication Therapy Management in geriatric
Medication Therapy Management (MTM)
Is a service provided typically by pharmacists that aims to improve outcomes by helping people to better understand their health conditions and the medications used to manage them.
Introduction
■ Geriatric patients: that individuals who are mainly 65 years or older in age.
■ Geriatric: refers to a branch of medicine focusing on management of health status and treatment of diseases in the older adult population.
■Elderly patients: usually present with more comorbidities, they often suffer from multiple disease, they commonly use more than a few medications. and they have physiologically deteriorated organ function due to the natural process of aging.
Important of MTM in geriatric Patients
■ The subsequent abuse of drugs, for the huge number of medications utilized for geriatric patients because of complicated illnesses and obstruction,
■ The rate of chronic diseases or conditions in geriatric is expanding, because of decline in organ function that occurs over time.
■ The potential for medication errors and harm associated with medication errors increases in the geriatric patient with a chronic disease or impairment.
Aim
The role of MTM provider to geriatric patient to reduce the rate of adverse drug event caused by medication errors, drug interactions.
Example for diseases in geriatric patients
- Hart failure
- Dyslipidemia
- Parkinson diseases
- Hypertension
Core Element for geriatric MTM
MTR: Medication Therapy Review
- Interview Patient to gather information for the appointment session
PMR: Patient Medication Record
- Generate a comprehensive report from the computer system
MAP: Medication-related Action Plan
- A Patient-centred document containing a list of actions for the patient to use in tracking progress for self-management
IAR: Intervention and Referral
- Consultative service and pharmacist interventions to address medication –related problems
DOC: Documentation and follow-up
- MTM services are documented and communicated to each prescriber and patient in a consistent manner.
Core 1. Medication Therapy Review (MTR)
■ A list of suggested questions to use when conducting a medication therapy review in a geriatric patient.
■ The number and types of questions will depend on several factors, including:
* Amount of time for the interview,
* Number of concurrent medication-related problems,
* Reliability of the patient in providing accurate information.
■ The MTM providers should gather the accompanying data: Detection and management of symptoms.
overall drug use and compliance;
the existence of extra risk factors for Increasing age ;
as well as prevention measures and evaluation of how to cope with emergency situations.
■ The MTM provider may choose to target questions that help to identify or rule out issues of an urgent nature.
■ MTM providers should remember to use simple language during the interview, and to be prepared for questions that patients may ask regarding geriatric issues.
■ Questions to Ask When Conducting a Medication Review in a geriatric Patients:
* What medication do you take at home?
* What is each medicine for?
* What is the dose?
* What medications do you take every day?
* What medication do you occasionally take?
* When do you take your medication?
* Have you recently started, stopped, or changed the medication you take?
* What medication are prescribed by any specialists you may see?
* What medication do you take that do not require a prescription?
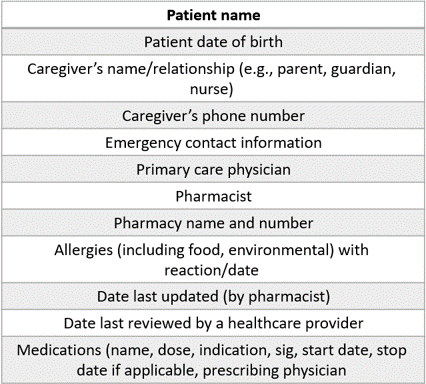
Core 2. Personal Medication Record (PMR)
The main Components of a Personal Medication Record.

Core 3. Medication related Action Plan (MAP)
■ MAP reiterates what was discussed with the patient about his disease and its management and identifies actions that the patient needs to take:
■ For example: medication adherence. – patients record what they did and when they took action.
Core 3. Medication related Action Plan (MAP)
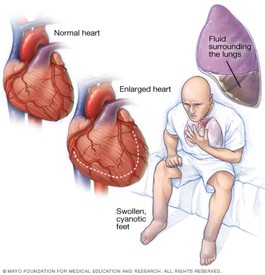
Heart failure as Example
■ HF is a progressive clinical syndrome that can result from any abnormality in cardiac structure or function that impairs the ability of the ventricle to fill with or eject blood.
■ Geriatric patient with HF can be managed by MTM provider as long as the treatment plan is followed, and follow-up visits are made.
■ Referral to a cardiology clinic is appropriate when:
Patient suffer from sign and symptoms, as indication his case is worsen: Dyspnea, Cough, Fatigue, weakness, Reduction in exercise capacity, or if patient has increasing in body weight
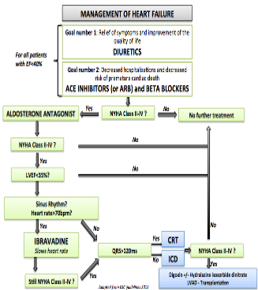
Core 3. Medication related Action Plan (MAP)
■ Diuretics:
Is the first line for management of HF.
It recommended for all patients with EF<40%.
It work as relief of symptoms and improvement of quality of life.
■ Diuretics Monitor:
To avoid hypotension, monitor blood pressure carefully.
Electrolyte abnormalities are more likely and must be monitored closely.
Avoid combination with another ototoxic med if possible.
Diuretics can decrease renal clearance of lithium and increase risk of lithium toxicity.
Core 3. Medication related Action Plan (MAP)
Parkinson’s disease
■ Is a progressive nervous system disorder that affects movement. Symptoms start gradually, sometimes starting with a barely noticeable tremor in just one hand.
■ Tremors are common, but the disorder also commonly causes stiffness or slowing of movement.
■ Parkinson’s disease symptoms worsen as patient condition progresses over time.
■ Therapies for PD is related to slow the progression or provide a neuroprotective effect, So, the Appropriate management requires an evaluation by a MTM provider for the therapeutic outcome and medication adherence.
■ Referral to a neurology clinic is appropriate when: the symptoms is progress
■ Three main types of medication are commonly used:
- levodopa
- dopamine agonists
- monoamine oxidase-B inhibitors
■ MTM provider can explain your medication options, including the risks associated with each medication, and discuss which may be best.
■ Regular reviews will be required as the condition progresses, and patient needs change.
Core 4-Intervention and/or Referral
1.■ clinical pharmacy services review of treatment chart for appropriate indications drug dosing, dosage form, drug duplication, drug interactions, and drug allergies.
2.■ MTM provider plays an important role in identifying, reporting, investigating, and preventing all types of medication errors and adverse drug reactions (ADRs).
3.■ Other interventions include correction and clarification of physician orders, providing drug and poison information, and recommending an alternative therapy.
4.■ Clinical pharmacist adjusts dose of drugs in pediatric, geriatric, renal, and hepatic failure patients.
5.■ Pharmacist also involved in optimizing antibiotic usage based on patient characteristics, site of infection, pharmacokinetics, dose adjustment, and de-escalation.
6.■ Clinical pharmacist also contributes to continuing education activities through teaching programs for doctors and nurses. This increases direct patient care practice abilities, creates awareness among intensive care team, and prevents medication errors.
Core 5. Documentation and Follow-Up
Proper documentation of MTM services may serve several purposes including, but not limited, to the following:
■ Facilitating communication between the pharmacist and the patient’s other healthcare professionals regarding recommendations intended to resolve or monitor actual or potential medication-related problems
■ Improving patient care and outcomes
■ Enhancing the continuity of patient care among providers and care settings
■ Ensuring compliance with laws and regulations for the maintenance of patient records
■ Protecting against professional liability
■ Capturing services provided for justification of billing or reimbursement (e.g., payer audits)
■ Demonstrating the value of pharmacist-provided MTM services
■ Demonstrating clinical, economic, and humanistic outcomes
■ Once patient is alert, explain why drug was given.
■ Reassure patient he will be monitored continuously until he is stable.
■ If the patient will be remaining in the same care setting, the pharmacist should arrange for consistent follow-up MTM services in accordance with the patient’s unique medication-related needs.
■ All follow-up evaluations and interactions with the patient and his or her other healthcare professional should be included in MTM documentation.
should be include the following:
■ Name, strength, and description of such tablet.
■ Frequency of dose and administration time.
■ How to handle missed doses.
■ Purpose of heart failure therapy and how it works.
■ Medications/supplements and dietary interactions.
■ Recognition of symptoms of adverse reactions and the appropriate procedures to follow.
■ Importance of compliance with treatment and clinic appointments.
■ Educate patients on the use of treatment during pregnancy or lactation if necessary
RESOURCES
- Anderson Sl, Marrs Jc. a review of the role of the pharmacist in heart failure transition of care. adv ther. 2018;35(3):311-323. doi:10.1007/s12325-018-0671-7
- Thomas M. Maddox, MD, Msc, FACC Chair James L. Januzzi, Jr., MD, FACC Vice Chair Larry A. Allen, MD, MHS, FACC Khadijah Breathett, MD, MS, FACC Javed Butler, MD, MBA, MPH, FACC Leslie L. Davis, Phd, RN, ANP-BC, FACC Gregg C. Fonarow, MD, FACC Nasrien E. Ibrahim, MD, FACC Joann Lindenfeld, MD, FACC Frederick A. Masoudi, MD, MSPH, FACC Shweta R. Motiwala, MD, MPH Estefania Oliveros, MD, MscJ. Herbert Patterson, PharmdMary Norine Walsh, MD, MACC Alan Wasserman, MD, FACC Clyde W. Yancy, MD, Msc, MACC Quentin R. Youmans. 2021 update to the 2017 acc expert consensus decision pathway for optimization of heart failure treatment: answers to 10 pivotal issues about heart failure with reduced ejection fraction: a report of the american college of cardiology solution set oversight committee. J Am Coll Cardiol. 2021 Feb, 77 (6) 772–810
- Azad N, Lemay G. management of chronic heart failure in the older population. J Geriatr Cardiol. 2014;11(4):329-337. doi:10.11909/j.issn.1671-5411.2014.04.008
Read More:
- 10 Skills You Must Learn to Do Research via Google Scholar
- Register Now at FADIC Clinical Research School
- Buy FADIC Toolkit for Writing Research to Write a Great Research Paper
- Read 10 Skills You Must Learn to Do Research via Google Scholar in Arabic
- The FADIC Online Continuous Medical Improvement Programs & Mini-Courses.
- Check Now the FADIC Book store and Buy books in different specialities.
- Check Now about Coronavirus Resource Information Center.
- Simple random sampling: Definition, examples, and how to do it

 Log in
Log in Sign up
Sign up