Respiratory Patient Counseling
Respiratory Patient Counseling

What is the respiratory disease?
Respiratory disease is a medical term that encompasses pathological conditions affecting the organs and tissues that make gas exchange.
It includes conditions of the upper respiratory tract, trachea, bronchi, bronchioles, alveoli, pleura and pleural cavity, and the nerves and muscles of breathing.
Respiratory diseases range from mild and self-limiting, such as the common cold, to life-threatening like pneumonia, acute asthma and lung cancer.
Most common respiratory illness
The top eight respiratory system illnesses that require Respiratory Patient Counseling include:
- Asthma
- Chronic Obstructive Pulmonary Disease (COPD)
- Chronic Bronchitis
- Emphysema
- Lung Cancer
- Cystic Fibrosis/Bronchiectasis
- Pneumonia
- Pleural Effusion
- Preventative Measures for Respiratory Disease
-
Highly recommend online Marketing tool from SEMRUSH
Asthma patient counseling
-
What is Asthma
Asthma is a disease that affects your lungs.
It causes repeated episodes of wheezing, breathlessness, chest tightness, and nighttime or early morning coughing.
-
Pathophysiology of Asthma
Asthma is a chronic disease of the airways that makes breathing difficult.
With asthma, there is inflammation of the air passages.
This results in a temporary narrowing of the airways that carry oxygen to the lungs which causes asthma symptoms.
Asthma involves many pathophysiologic factors.
These include bronchiolar inflammation with airway constriction and resistance that manifests as episodes of coughing, shortness of breath, and wheezing.
Moreover, the Asthma can affect the trachea, bronchi, and bronchioles.
Inflammation can exist even though obvious signs and symptoms of asthma may not always occur.
Asthma is considered the most chronic disease in childhood and affects an estimated 7 million children.
Besides, Two-thirds of all asthma cases are diagnosed before patients who are 18 years of age.
An estimated 50% of pediatric patients diagnosed with asthma often see a disappearance of symptoms by early adulthood.
-
Symptoms of asthma
People with asthma experience symptoms when the airways tighten, become inflamed, or fill with mucus.
Common symptoms of asthma include:
- Frequent coughing
- Trouble sleeping due to coughing and wheezing
- Wheezing
- Shortness of breath or trouble breathing
- Pain or tightness in the chest

-
Triggers of asthma “Counseling Guide for Avoiding Asthma Triggers”
Asthma symptoms often occur in response to a trigger. Common triggers include:
-
Tobacco Smoke
Tobacco smoke is unhealthy for everyone, especially people with asthma.
Moreoever, If you have asthma and you smoke, quit smoking.
Secondhand smoke can trigger an asthma attack.
If you have asthma, people should never smoke near you.
-
Dust Mites
Dust mites are tiny bugs that are in almost every home.
If you have asthma, dust mites can trigger an asthma attack.
In addition to prevent attacks, use mattress covers and pillowcase covers to make a barrier between dust mites and yourself.
-
Outdoor Air Pollution
Outdoor air pollution can trigger an asthma attack.
Moreover, This pollution can come from factories, cars, and other sources.
Pay attention to air quality forecasts on radio, television, and the Internet.
Try to plan your activities for when air pollution levels will be low.
-
Cockroach Allergen
Cockroaches and their droppings can trigger an asthma attack.
In addition to get rid of cockroaches in your home by removing as many water and food sources as you can.
At least every 2 to 3 days, vacuum or sweep areas that might attract cockroaches.
-
Furry pets
They can trigger an asthma attack.
If you think a furry pet may be causing attacks, you may want to find the pet another home.
Bathe pets every week and keep them outside as much as you can
-
Mold
Breathing in mold can trigger an asthma attack.
Get rid of mold in your home to help control your attacks.
Moreover, Humidity, the amount of moisture in the air, can make mold grow.
An air conditioner or dehumidifier will help you keep the humidity level low.
-
Smoke From Burning Wood or Grass
Smoke from burning wood or other plants is made up of a mix of harmful gases and small particles.
In addition to Breathing in too much of this smoke can cause an asthma attack.
If you can, avoid burning wood in your home.
-
Other Triggers
Infections linked to influenza (flu), colds, and respiratory syncytial virus (RSV) can trigger asthma.
Moreover, Sinus infections, allergies, breathing in some chemicals, and acid reflux can also trigger attacks.
Physical exercise; some medicines; bad weather, such as thunderstorms or high humidity.
In addition to breathing in cold, dry air; and some foods, food additives, and fragrances.

-
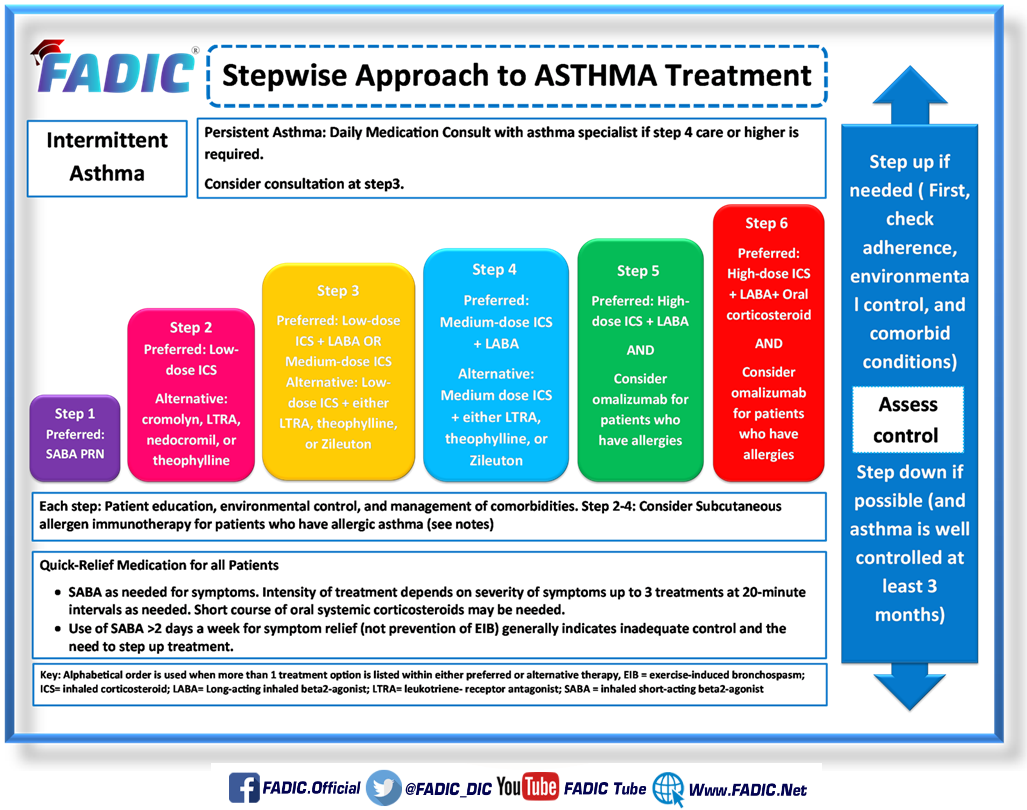
Asthma Severity & treatment
Asthma may be classified as intermittent, mild persistent, moderate persistent and severe persistent.
The severity is judged based on:
- how much your symptoms affect your life
- how well your lungs work
- the risk of having an asthma attack and death

Treatment:
Prevention and long-term control are key in stopping asthma attacks before them start.
In addition to the Treatment usually involves learning to recognize your triggers, taking steps to avoid them.
Moreover, tracking your breathing to make sure your daily asthma medications are keeping symptoms under control.
In case of an asthma flare-up, you may need to use a quick-relief inhaler, such as albuterol.
Medication:
Long-term asthma control medications
They are generally taken daily and considered the cornerstone of asthma treatment.
These medications keep asthma under control on a day-to-day basis and make it less likely you’ll have an asthma attack.
Types of long-term control medications include:
-
Inhaled corticosteroids:
These anti-inflammatory drugs include
- Fluticasone (Flonase, Flovent HFA)
- Budesonide (Pulmicort Flexhaler, Rhinocort)
- Flunisolide (Aerospan HFA)
- Ciclesonide (Alvesco, Omnaris, Zetonna), beclomethasone (Qnasl, Qvar)
- Mometasone (Asmanex)
- Fluticasone furoate (Arnuity Ellipta)
You may need to use these medications for several days to weeks before they reach their maximum benefit.
Unlike oral corticosteroids, these corticosteroid medications have a relatively low risk of side effects and are generally safe.

How to use a corticosteroid inhaler?
There are two different types of corticosteroid inhalers:
Most metered dose inhalers spray medicine when you press down on the top of the canister.
In addition to some metered dose inhalers are meant to be used with a spacer.
A spacer is a device that attaches to the inhaler’s mouthpiece
When you press down on the canister, the medicine sprays into the spacer and sits there until you breathe it in.
Your doctor or nurse will tell you if you should use a spacer with your corticosteroid inhaler.
-
Dry powder inhalers
These release medicine when you take a deep breath in from the inhaler.
Most people take 1 or 2 puffs from their inhaler in the morning and 1 or 2 puffs in the evening.
Inhaled corticosteroids can only work to prevent breathing problems if you use your inhaler every day, even when you are not having trouble breathing.
What should I know about inhaled corticosteroids?
These are some things to keep in mind:
- A steroid inhaler helps prevent breathing problem flare ups.
It does not relieve symptoms quickly.
Your doctor will prescribe a different kind of inhaler to help quickly relieve breathing problems, such as asthma or COPD “attacks.” - It’s important to keep using your steroid inhaler every day as your prescription says, even if you feel well.
- Gargle and rinse your mouth with water and spit it out or brush your teeth after you use your steroid inhaler.
- If you are not sure how to use your inhaler or spacer correctly, talk to your doctor, nurse, or pharmacist.
- Inhaled corticosteroids are usually considered safe to use during pregnancy and breastfeeding, but it’s best to review this with your doctor firs
-
Leukotriene modifiers:
These oral medications include:
- Montelukast (Singulair)
- Zafirlukast (Accolate)
- Zileuton (Zyflo)
They help relieve asthma symptoms for up to 24 hours.
What should I know about these drugs:
- Do not use this drug to treat an asthma attack.
Use a rescue inhaler. - Call your doctor right away if your breathing problems get worse, if your rescue inhaler does not work as well, or if you need to use your rescue inhaler more often.
- If you take this drug for asthma or allergy, do not take another dose to prevent exercise-induced breathing problems.
- Additionally, if you have asthma and taking aspirin makes it worse, keep avoiding aspirin and NSAIDs while you take this drug.
- Besides, if you are switching to this drug from a steroid, do not stop taking the steroid all of a sudden.
The dose of the steroid may need to be slowly lowered to avoid side effects.

They are inhaled medications includeLong-acting beta agonists:
- Salmeterol (Serevent)
- Formoterol (Foradil, Perforomist)
Some research shows that they may increase the risk of a severe asthma attack, so take them only in combination with an inhaled corticosteroid.

What should I know about these drugs
- Tell all of your health care providers that you take this drug.
- If you have high blood sugar (diabetes), this drug may sometimes raise blood sugar.
- Do not take more of this drug or use it more often than you have been told.
Deaths have happened when too much of this type of drug has been taken. - If you are 65 or older, use this drug with care. You could have more side effects.
- Tell your doctor if you are pregnant or plan on getting pregnant.
- Tell your doctor if you are breast-feeding.
- Combination inhalers:
These medications contain a long-acting beta agonist along with a corticosteroid such as
- Fluticasone-salmeterol (Advair Diskus)
- Budesonide-formoterol (Symbicort)
- Formoterol-mometasone (Dulera)
In addition to these inhalers contain long-acting beta agonists, they may increase your risk of having a severe asthma attack.

What should I know about these drugs
- Tell all of your health care providers that you take this drug.
- If you have high blood sugar (diabetes).
This drug may raise blood sugar. - It may take 2 weeks to see the full effect.
- Do not take more of this drug or use it more often than you have been told.
- When changing from an oral steroid to another form of a steroid, there may be very bad and sometimes deadly side effects.
- Long-term use may raise the chance of cataracts or glaucoma.
- Have an eye exam as you have been told by your doctor.
- This drug may cause weak bones (osteoporosis) with long-term use.
- You may have more chance of getting an infection. Wash hands often. Stay away from people with infections, colds, or flu.
- If you are 65 or older, use this drug with care. You could have more side effects.
- This drug may affect growth in children and teens in some cases. They may need regular growth checks.
- Tell your doctor if you are pregnant or plan on getting pregnant.
-
Theophylline:
Theophylline (Theo-24, Elixophyllin) is a daily pill that helps keep the airways open (bronchodilator)
It relaxes the muscles around the airways.
Moreover, it’s not used as often now as in past years.
What should I know about this drug?
- Tell all of your health care providers that you take this drug.
- This drug may affect certain lab tests.
- Wear disease medical alert ID (identification).
- Have blood work checked as you have been told by the doctor.
- If you have high blood sugar (diabetes), you will need to watch your blood sugar closely.
- Limit your use of caffeine (for example, tea, coffee, cola) and chocolate.
- If you start or stop smoking tobacco or marijuana, talk with your doctor.
- If you get sick, have a fever, or have a long-term illness that gets worse, talk with your doctor.
- Some other drugs may affect how much of this drug is in your body.
- Tell your doctor if another doctor gives you a new drug or tells you to stop taking a drug you have been using.
- Use with care in children. Talk with the doctor.
-
Quick-relief (rescue) medications
They are used as needed for rapid, short-term symptom relief during an asthma attack
In addition to the types of quick-relief medications include:
-
Short-acting beta agonists:
These inhaled, quick-relief bronchodilators act within minutes to rapidly ease symptoms of an asthma attack.
They include:
- Albuterol (ProAir HFA, Ventolin HFA, others)
- Levalbuterol (Xopenex)
What should I know about this drugs?
- Tell all of your health care providers that you take this drug.
- Do not take more of this drug or use it more often than you have been told.
- Call your doctor right away if your normal dose does not work well, if your signs get worse, or if you need to use this drug more often than normal.
- If you have high blood sugar (diabetes), you will need to watch your blood sugar closely.
- If you are taking digoxin, talk with your doctor.
You may need to have your blood work checked more closely
-
Ipratropium (Atrovent):
Like other bronchodilators, ipratropium acts quickly to immediately relax your airways, making it easier to breathe.
Ipratropium is mostly used for emphysema and chronic bronchitis, but it’s sometimes used to treat asthma attacks.
What should I know about this drug?
- Tell all of your health care providers that you take this drug.
- Avoid driving and doing other tasks or actions that call for you to be alert or have clear eyesight until you see how this drug affects you.
- Call your doctor right away if your breathing problems get worse, if your rescue inhaler does not work as well, or if you need to use your rescue inhaler more often.
- If this drug gets in the eyes, rinse with water right away.
- Call the doctor right away if this drug gets in the eyes and blurred eyesight, worsened glaucoma, or eye pain happens.
- Tell your doctor if you are pregnant or plan on getting pregnant
-
Oral and intravenous corticosteroids:
These medications — which include prednisone and methylprednisolone — relieve airway inflammation caused by severe asthma.
In addition to they are used only on a short-term basis to treat severe asthma symptoms.
If you have an asthma flare-up, a quick-relief inhaler can ease your symptoms right away.
But if your long-term control medications are working properly, you shouldn’t need to use your quick-relief inhaler very often.

-
Asthma patient education
Patients and their families must be prepared to make lifestyle changes and adhere to drug therapy for long periods.
Moreover, they must be capable of making rapid decisions about self-medication and the need to seek medical advice.
During counseling, patients and caregivers of children with asthma should be educated on
- the basics of asthma.
- The goals of treatment
- how to manage triggers
- how to properly use metered-dose inhalers
- the importance of adhering to therapy
- refilling prescriptions on time
- carrying rescue medications at all times because attacks may occur without warning
- how to use maintenance and rescue medications.
Because patients with asthma are at an increased risk for developing respiratory complications from infections such as influenza and pneumonia.
Patients should be encouraged to obtain a yearly inactivated influenza vaccination.
Although asthma is a chronic condition, it can be successfully managed through patient education and adherence
With effective therapy, patients can lead normal, healthy lives.
-
Types of Inhalers, and How to use them?
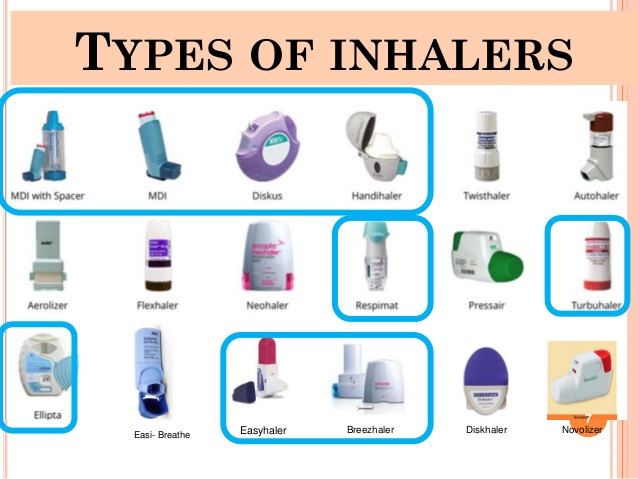
The three main types of inhaler devices for asthma and COPD medicines are:
- manually-actuated pressurised metered-dose inhalers (conventional puffer)
- breath-actuated pressurised metered-dose inhalers
- dry powder inhalers (multi-dose and capsule types)
- mist inhalers.
Steps to correctly use your inhaler:
- Remove the cap and hold the inhaler upright.
- Shake the inhaler.
- Tilt your head back slightly and breathe out.
- If your doctor recommends, use a spacer (a hollow, plastic chamber) to filter the medicine between the inhaler and your mouth.
- The chamber protects your throat from irritation from the medicine. Check your insurance plan, as not all insurers offer coverage for spacers.
- Press down on the inhaler to release the medicine as you start to breathe in slowly.
- Breathe in slowly for 3 to 5 seconds.
- Hold your breath for 10 seconds to allow medicine to go deeply into your lungs.
- Repeat puffs as directed. Wait 1 minute between puffs to allow the second puff to get into the lungs better.
These instructions are for a metered-dose inhaler only. Inhaled dry powder capsules are used differently.
In addition to use a dry powder inhaler, close your mouth tightly around the mouthpiece of the inhaler and breathe in quickly.
-
The Pharmacist’s Role in Asthma
The role of pharmacists in treating asthma is huge.
In addition to optimising outcomes in patients with asthma requires vigilance and clinical judgment.
When treating both children and adults coping with asthma, it’s important to
- repeat patient counseling and technique assessment
- make the best therapy choices
- get rid of factors that worsen symptoms.
Pharmacists are instrumental in providing patients with valuable resources to educate them about treating and managing asthma.
Moreover, the pharmacists can use their knowledge and time to educate patients and prescribers to decrease patients’ symptoms and.
In addition to, the pharmacists often educate patients about the proper use of inhalers, especially newly diagnosed patients.
For successful management of asthma, it is important that patients be thoroughly educated about
- their condition
- Besides, know the warning signs of asthma attacks
- Moreover, know the factors that may trigger an attack,
- know how to manage attacks
- adhere to their asthma plan
- know how to properly use the prescribed treatment.
Increasing awareness and promoting education about asthma can reduce the numbers of asthma-related hospitalisations.

COPD patient counseling and Education
-
Pathophysiology of COPD
Chronic obstructive pulmonary disease (COPD) is a chronic inflammatory lung disease that causes obstructed airflow from the lungs.
In addition to chronic inflammation plays a major role in COPD pathophysiology.
Smoking and other airway irritants cause neutrophils, T-lymphocytes, and other inflammatory cells to accumulate in the airways.
Once activated, they trigger an inflammatory response in which inflammatory mediators navigate to the site in an attempt to destroy and remove inhaled foreign debris.
Repeated exposure to airway irritants perpetuates an ongoing inflammatory response that never seems to shut itself off.
As inflammation continues, the airways constrict, becoming excessively narrow and swollen.
This leads to excess mucus production and poorly functioning cilia.
When people with COPD can’t clear their secretions, they develop symptoms of COPD, including a chronic productive cough, wheezing, and dyspnea.
What Are the Symptoms and Risk Factors?
Symptoms :
COPD symptoms often don’t appear until significant lung damage has occurred.
They usually worsen over time, particularly if smoking exposure continues.
For chronic bronchitis, the main symptom is a daily cough and mucus (sputum) production
Other signs and symptoms of COPD may include:
- Shortness of breath, especially during physical activities
- Wheezing
- Chest tightness
- Having to clear your throat first thing in the morning, due to excess mucus in your lungs
- A chronic cough that may produce mucus (sputum) that may be clear, white, yellow or greenish
- Blueness of the lips or fingernail beds (cyanosis)
- Frequent respiratory infections
- Lack of energy
- Unintended weight loss (in later stages)
- Swelling in ankles, feet or legs
Risk factors
Risk factors for COPD include:
- Exposure to tobacco smoke.
The most significant risk factor for COPD is long-term cigarette smoking.
The more years you smoke and the more packs you smoke, the greater your risk..
- People with asthma who smoke.
The combination of asthma, a chronic inflammatory airway disease, and smoking increases the risk of COPD even more.
- Occupational exposure to dusts and chemicals.
Long-term exposure to chemical fumes, vapors and dusts in the workplace can irritate and inflame your lungs.
- Exposure to fumes from burning fuel.
COPD develops slowly over years, so most people are at least 40 years old when symptoms begin.
The uncommon genetic disorder alpha-1-antitrypsin deficiency is the cause of some cases of COPD.
Management of COPD
The main goals of COPD treatment:
- Relieve your symptoms
- Slow your decline in lung function
- Improve your daily lung function
- Decrease your number of acute episodes (called COPD exacerbations(
- Improve your overall quality of life
Here are some of the treatments of COPD:

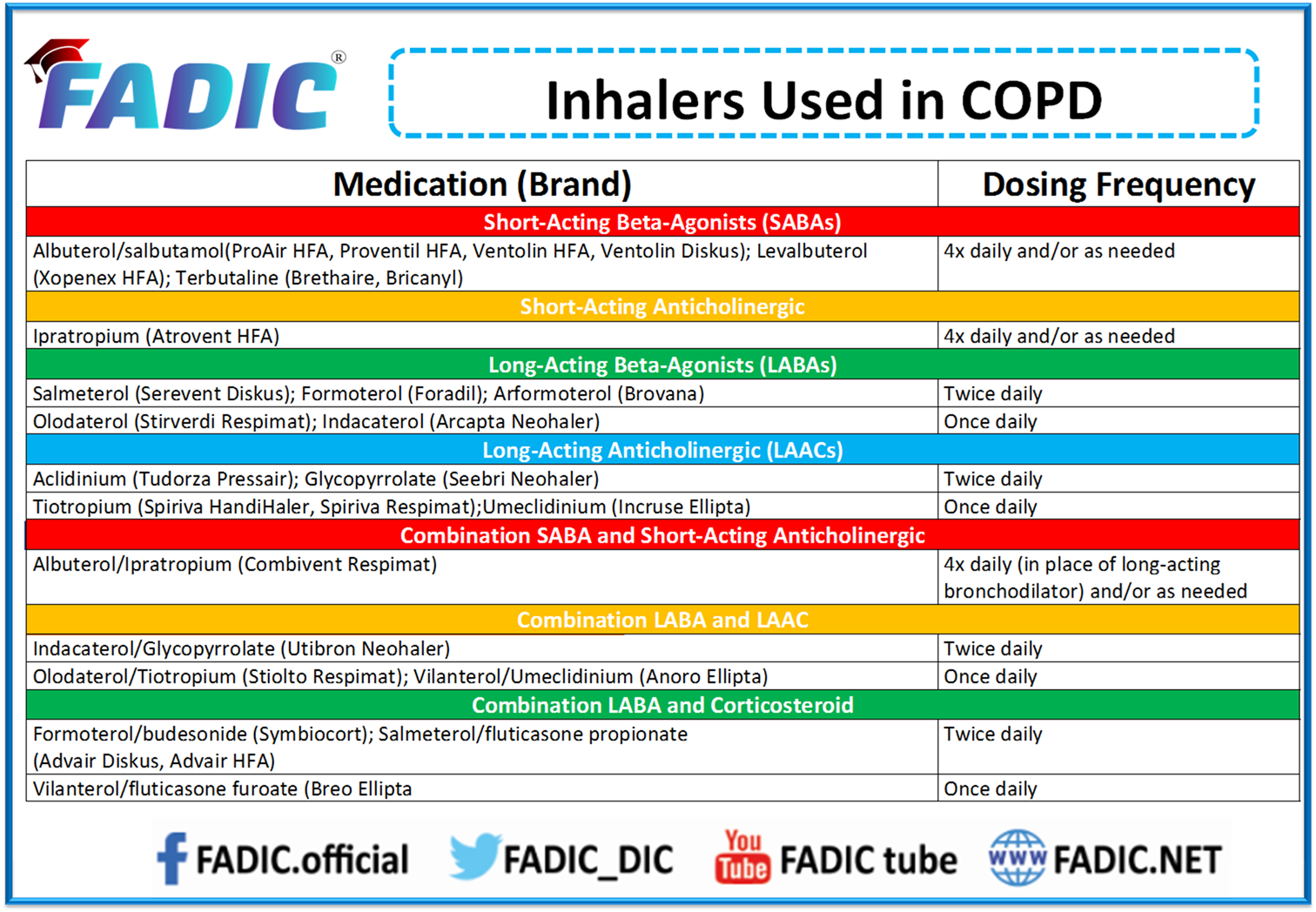
Bronchodilators
These relax the muscles around your airways to let more air into your lungs.
They can help with symptoms such as a cough and shortness of breath.
You breathe the medicine into your lungs through a device called an inhaler.
- Bronchodilators can be short-acting or long-acting:
- Short-acting bronchodilators:
These work quickly, and the effects last for about 4 to 6 hours.
These drugs are helpful for people who only have symptoms from time to time.
Short-acting bronchodilators may include:
- Albuterol (ProAir HFA, Ventolin HFA)
- Levalbuterol (Xopenex HFA)
- Ipratropium (Atrovent)
- Ipratropium bromide and albuterol (Combivent)
Long-acting bronchodilators:
They work for up to 12 hours.
You take these every day to prevent symptoms.
Some of them are:
- Aclidinium (Tudorza Pressair)
- Arformoterol (Brovana)
- Formoterol (Foradil, Performist)
- Indacaterol (Arcapta)
- Salmeterol (Serevent)
- Tiotropium (Spiriva)
Steroids
These bring down swelling in your airways.
You usually breathe them in through an inhaler.
Inhaled steroids can help if you have many COPD flare-ups. You might take steroids as a pill if your symptoms get worse.
Examples of inhaled steroids are:
- Budesonide (Entocort, Pulmicort, Uceris)
- Fluticasone (Cutivate, Flovent HFA, Flonase)
What should I know about these drugs:
- Tell all of your health care providers that you take this drug.
- You may have more chance of getting an infection. Wash hands often.
- If you have high blood sugar (diabetes), you will need to watch your blood sugar closely.
- If your normal short-acting inhaler dose does not work well, you need to use your short-acting inhaler more often than normal, or your breathing gets worse, call your doctor right away.
- This drug is not helpful during an asthma attack.
- When changing from an oral steroid to another form of a steroid, there may be very bad and sometimes deadly side effects.
- If you have been taking this drug for many weeks, talk with your doctor before stopping.
- This drug may cause weak bones (osteoporosis) with long-term use.
- Have a bone density test as you have been told by your doctor.
- Long-term use may raise the chance of cataracts or glaucoma.
- Have your eye pressure checked if you are on this drug for a long time.
- If you are 65 or older, use this drug with care.
- This drug may affect growth in children and teens in some cases. They may need regular growth checks.
Some medicines combine a bronchodilator and inhaled steroid. These include:
- Budesonide and formoterol (Symbicort(
- Futicasone and salmeterol (Advair)
-
Oxygen Therapy
Severe COPD can prevent you from getting enough air into your lungs.
As a result, oxygen levels in your blood can get too low.
Therapy increases these levels to help you stay active and healthy.
Lifestyle Changes to Help Manage COPD
-
Quitting Smoking
COPD and smoking are a deadly combination.
If you only do one thing to manage your COPD, quit smoking.
Smoking not only leads to COPD, but it speeds up the progress of the disease.
-
Defend against infections
People with COPD are at an increased risk for respiratory infections, which can trigger flare-ups.
Infections that affect the airways can often be avoided with good hand-washing hygiene.
It may also be helpful to avoid contact with people who show signs of cold or flu.
Your doctor may also recommend an annual flu vaccine.
-
Focus on good nutrition
Eating right is an important way to keep your body and your immune system strong.
Sometimes, people with advanced COPD don’t get the proper nutrition they need to stay healthy.
It may be helpful to eat smaller meals more often.
- Stay active and physically fit
Exercise training can improve exercise tolerance and improve quality of life among people with mild to moderate COPD.
The Pharmacist’s Role in the Management of COPD
Pharmacists should encourage COPD patients to stop smoking immediately and recommend medications to help facilitate the discontinuation of smoking.
Research has shown that brief counseling of 3 minutes results in quit rates of 5% to 10%.
Nicotine replacement therapy includes nicotine gum, inhaler, nasal spray, transdermal patch, sublingual tablet, or lozengs.
COPD patients should be educated about flu and pneumonia prevention.
Influenza and pneumococcal vaccines help to decrease the risk of COPD exacerbations and are recommended for all patients with COPD
Inhalers are the COPD patient’s constant companion.
Common treatments for COPD include inhalers that deliver either a bronchodilator or an inhaled corticosteroid.
Pharmacists need to review inhaler technique with patients regularly.
Conclusion
Asthma and COPD are of the most common respiratory diseases.
There are many treatments for both diseases.
Pharmacist patient counseling plays an important role in the management and control of Asthma and COPD.
Read More
- Check Now Updated FADIC articles through English FADIC Blog
- Join Now FADIC School of Antimicrobial Stewardship to learn how to apply antimicrobial stewardship.
- FADIC News Network “FNN” send every business day an email with the news/updates of the day
- Podcast of FADIC, help you to learn from others experience in the clinical practice.
- It is now time to share into publication process, Join FADIC School of Research.
- Check Now The Latest of FADIC Events
- Register Now in FADIC® – Online Programs & Mini-Courses and Stay Updated
- Enroll NOW in FADIC Patient Counseling and Education Program
- Download Now the Info-graphic of Patient Centered-Care, from this LINK.

 Log in
Log in Sign up
Sign up