Sepsis
Sepsis
Updates in the Management of Sepsis and Septic Shock

What is Sepsis?
- Sepsis is a life-threatening illness caused by your body’s response to an infection.
- Your immune system protects you from many illnesses and infections, but it’s also possible for it to go into overdrive in response to an infection.
- Sepsis is the body’s extreme response to an infection.
- It is a life-threatening medical emergency.
- The Sepsis happens when an infection you already have triggers a chain reaction throughout your body.
- Without timely treatment, sepsis can rapidly lead to tissue damage, organ failure, and death.
- Almost any type of infection can lead to sepsis.
- Infections that lead to sepsis most often start in the lung, urinary tract, skin, or gastrointestinal tract.
- There are more than 1.5 million cases of sepsis each year, according to the Centers for Disease Control and Prevention (CDC)
Sepsis Pathophysiology
Malignant intravascular inflammation
- Sepsis has been referred to as a process of malignant intravascular inflammation.
- Normally, a potent, complex, immunologic cascade ensures a prompt protective response to microorganism invasion in humans.
- A deficient immunologic defense may allow infection to become established; however, an excessive or poorly regulated response may harm the host through maladaptive release of indigenously generated inflammatory compounds.
- Lipid A and other bacterial products release cytokines and other immune modulators that mediate the clinical manifestations of sepsis.
- Interleukins, tumor necrosis factor (TNF)-α, interferon gamma (IFN-γ), and other colony-stimulating factors are produced rapidly within minutes or hours after interactions of monocytes and macrophages with lipid A.
- Inflammatory mediator release becomes a self-stimulating process, and release of other such mediators, including interleukin (IL)-1, platelet activating factor, IL-2, IL-6, IL-8, IL-10, and nitric oxide (NO), further increases cytokine levels.
- This leads to continued activation of polymorphonuclear leukocytes (PMNs), macrophages, and lymphocytes; proinflammatory mediators recruit more of these cells.
- All of these processes create a state of destructive immunologic dissonance.
- Organ dysfunction or organ failure may be the first clinical sign of sepsis, and no organ system is immune from the consequences of the inflammatory excesses of sepsis.
- Mortality increases as organ failure increases.
- Survival from severe sepsis requires a generalized down-regulation of the body’s immune response, energetic functions, and associated organ performance.
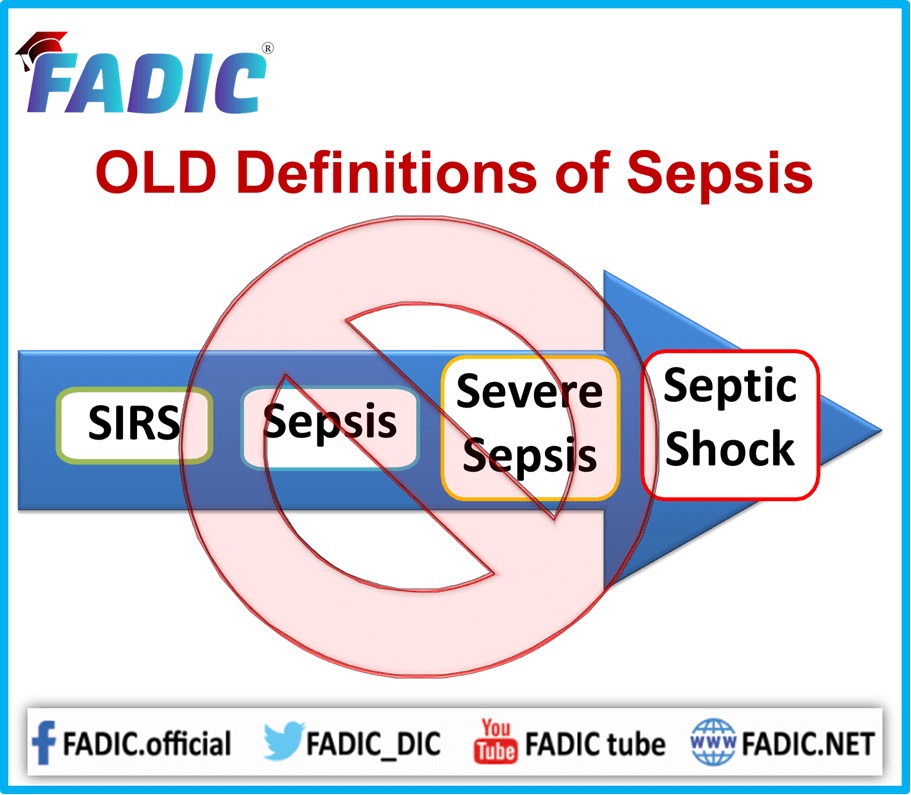
Stages of Sepsis
There are three stages of sepsis: sepsis, severe sepsis, and septic shock.
Sepsis
Symptoms of sepsis include:
- a fever above 101ºF (38ºC) or a temperature below 96.8ºF (36ºC)
- heart rate higher than 90 beats per minute
- breathing rate higher than 20 breaths per minute
- probable or confirmed infection
Severe Sepsis
Severe sepsis occurs when there’s organ failure. You must have one or more of the following signs to be diagnosed with severe sepsis:
- patches of discolored skin
- decreased urination
- changes in mental ability
- low platelet (blood clotting cells) count
- problems breathing
- abnormal heart functions
- chills due to fall in body temperature
- unconsciousness
- extreme weakness
Septic Shock
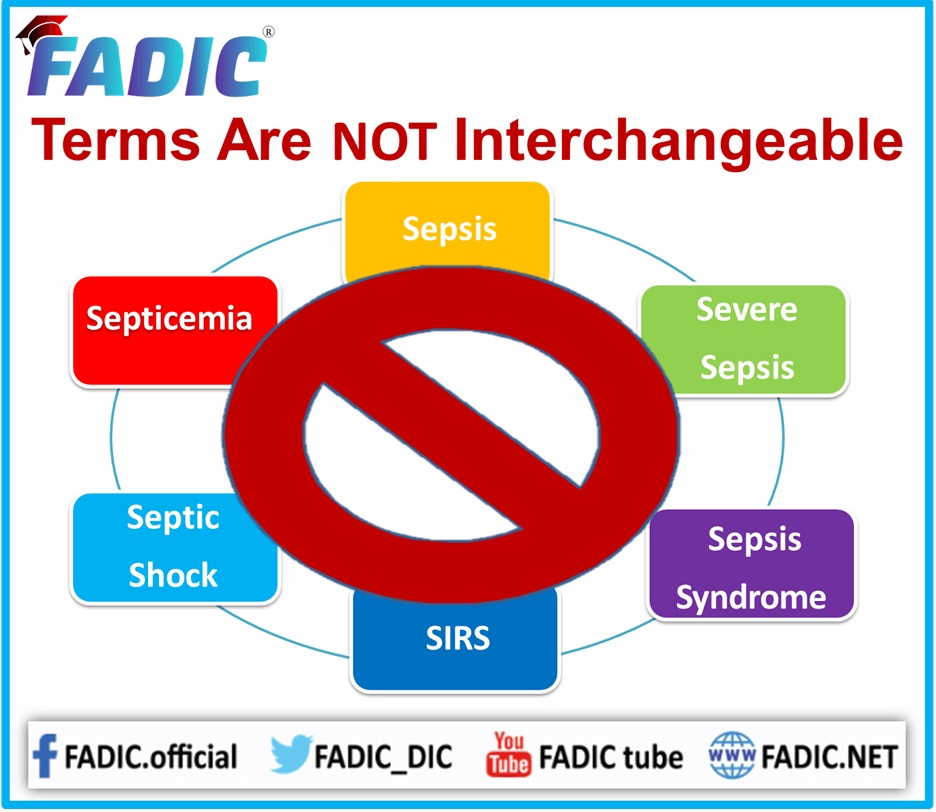
Symptoms of septic shock include the symptoms of severe sepsis, plus a very low blood pressure. The Differences between Sepsis and Septicemia
- Septicemia is a bacterial infection that spreads into the bloodstream.
- In the Sepsis, the body’s response to that infection, during which the immune system will trigger extreme, and potentially dangerous, whole-body inflammation.
- Moreover, Sepsis and septicemia are medical terms that refer to infections and your body’s response to those infections.
- The Sepsis and septicemia sometimes used interchangeably, but they’re not truly interchangeable—although the terms are closely related, their definitions are different.
Sepsis and Inflammation
- Sepsis is defined as an extreme inflammatory response to infection.
- Additionally, when body threatened with a severe infection your immune system responds by releasing chemical messengers to sound the alarm.
- These chemical messengers produce inflammation throughout your body.
- Moreover, the infection can be due to bacteria in the bloodstream, but sepsis can also be produced by an infection that is present only in one part of the body, such as the lungs in pneumonia.
- In addition to, the inflammation in sepsis can produce blood clots and leaking blood vessels. Without proper treatment, this can damage your organs and potentially kill you.
- Sepsis can progress to septic shock with your blood pressure dropping and your bodily systems starting to shut down.
- Moreover, the lungs, liver, and kidneys can fail.
- Therefore, sepsis is a medical emergency.
Septicemia and Infection - Septicemia is defined as having bacteria in the bloodstream that cause sepsis.
- Some people call septicemia “blood poisoning,” and this term is pretty accurate since the overwhelming bacterial infection can indeed poison your blood.
- Doctors no longer use the term septicemia much.
- Finally, to eliminate confusion surrounding like-sounding terms, they often use “sepsis” to refer to the inflammatory response and “bacteremia” to refer to the bacteria present in the bloodstream.
Symptoms of Sepsis
Because it can begin in different parts of your body, sepsis can have many different symptoms. The first signs may include rapid breathing and confusion. Other common symptoms include:
- Fever and chills
- Very low body temperature
- Peeing less than usual
- Fast heartbeat
- Nausea and vomiting
- Diarrhea
- Fatigue or weakness
- Blotchy or discolored skin
- Sweating or clammy skin
- Severe pain
Sepsis Causes and Risk Factors
Causes – While any type of infection — bacterial, viral or fungal — lead to sepsis, infections that more commonly result in sepsis include infections of:
- Lungs, such as pneumonia
- Kidney, bladder and other parts of the urinary system
- Digestive system
- Bloodstream (bacteremia)
- Catheter sites
- Wounds or burns
Risk factors – Several factors increase the risk of sepsis, including:
- Older age
- Infancy
- Compromised immune system
- Diabetes
- Chronic kidney or liver disease
- Admission to intensive care unit or longer hospital stays
- Invasive devices, such as intravenous catheters or breathing tubes
- Previous use of antibiotics or corticosteroids
Sepsis in Newborns
- Neonatal sepsis is a blood infection that occurs in an infant younger than 90 days old.
- Early-onset sepsis is seen in the first week of life. Late onset sepsis occurs after 1 week through 3 months of age.
Causes - Moreover, neonatal sepsis caused by bacteria such as Escherichia coli (E coli), Listeria, and some strains of streptococcus.
- Group B streptococcus (GBS) is a major cause of neonatal sepsis.
- However, this problem become less common because women are screened during pregnancy.
- Furthermore, the herpes simplex virus (HSV) can also cause a severe infection in a newborn baby.
- This happens most often when the mother newly infected.
- Early-onset neonatal sepsis most often appears within 24 to 48 hours of birth.
- Finally, the baby gets the infection from the mother before or during delivery.
Sepsis Symptoms
Infants with neonatal sepsis may have the following symptoms:
- Body temperature changes
- Breathing problems
- Diarrhea or decreased bowel movements
- Low blood sugar
- Reduced movements
- Reduced sucking
- Seizures
- Slow or fast heart rate
- Swollen belly area
- Vomiting
- Yellow skin and whites of the eyes (jaundice)
Exams and Tests of Sepsis
Lab tests can help diagnose neonatal sepsis and identify the cause of the infection. Blood tests may include:
- Blood culture
- C-reactive protein
- Complete blood count (CBC)
- In addition to, if a baby has symptoms of sepsis, a lumbar puncture (spinal tap) will be done to look at the spinal fluid for bacteria.
- Moreover, skin, stool, and urine cultures may be done for herpes virus, especially if the mother has a history of infection.
- A chest x-ray will be done if the baby has a cough or problems breathing.
- Urine culture tests are done in babies older than a few days.
Sepsis in Older Patients
- As we go through the aging process, our immune system becomes less effective at fighting infections.
- Additionally, this results in older people contracting more infections and they are more severe.
- As well, as people age, they may develop chronic illnesses, such as diabetes, COPD, kidney disease, or heart failure.
- It’s not unusual to see someone with two or more chronic diseases.
- Any type of infection can cause sepsis, from the flu to an infected bug bite, but the most common infections that trigger sepsis among older people are respiratory, such as pneumonia, or genitourinary, such as a urinary tract infection (UTI).
- In 2020, COVID-19 emerged as another strong risk factor for sepsis among older adults.
- Infections can also happen through infections in the mouth due to abscesses or other injuries, or skin sores, either from a simple skin tear because the skin may be dry or fragile, or a pressure injury from sitting in a wheelchair or lying in bed.
- Finally, since infections might not be obvious, if an older person becomes confused or behaves in an unusual manner, or if confusion or disorientation worsens, this could be a sign of an infection.
Symptoms of Sepsis in Adults:
Signs of sepsis are generally the same among all adults, regardless of age:
- Change in body temperature, either a fever (above 101.3 degrees F) or a lower than normal temperature (below 95 degrees F);
- Rapid heart rate (above 90 beats per minute);
- Rapid breathing (above 20 breaths per minute);
- Shaking
- Moreover, confusion, which may be more common among older people
- In addition to, sepsis can move into severe sepsis quickly, so getting help and treatment as quickly as possible is vital.
Why is sepsis so serious for people who are Aging?
- Sepsis is a very serious illness for anyone at any age, but it can be particularly devastating for seniors.
- Moreover, older severe sepsis survivors are more than three times more likely to see a drop in cognitive (mental) abilities that can make it impossible for them to return to their previous living arrangements.
- As well, the risk of dying from severe sepsis or septic shock rises as you get older.
Sepsis Diagnosis
According to the Surviving Sepsis Guidelines, a sepsis diagnosis requires the presence of infection, which can be proven or suspected, and 2 or more of the following criteria:
- Hypotension (systolic blood pressure < 90 mm Hg or fallen by >40 from baseline, mean arterial pressure < 70 mm Hg)
- Lactate > 1 mmol/L
- Mottled skin
- Decreased capillary refill of nail beds or skin
- Fever > 38.3 degrees C, or 101 degrees F
- Hypothermia < 36 degrees C core temperature (<96.8 degrees F)
- Heart rate > 90
- Tachypnea
- Change in mental status
- Significant edema or positive fluid balance (>20 mL/kg over 24 hours)
- Hyperglycemia (>140 mg/dL) in someone without diabetes
- White blood cell count > 12,000 or less than 4,000, or with >10% “bands” (immature forms)
- Elevated C-reactive protein in serum (according to your lab’s cutoffs)
- Elevated procalcitonin in serum (according to your lab)
- Arterial hypoxemia (paO2 / FiO2 < 300)
- Acute drop in urine output (<0.5 ml/kg/hr for at least 2 hours despite fluid resuscitation, or about 35 ml/hour for a 70 kg person)
- Creatinine increase > 0.5 mg/dL
- INR > 1.5 or aPTT > 60 seconds
- Absent bowel sounds (ileus)
- Platelet count < 100,000
- High bilirubin (total bilirubin > 4 mg/dL
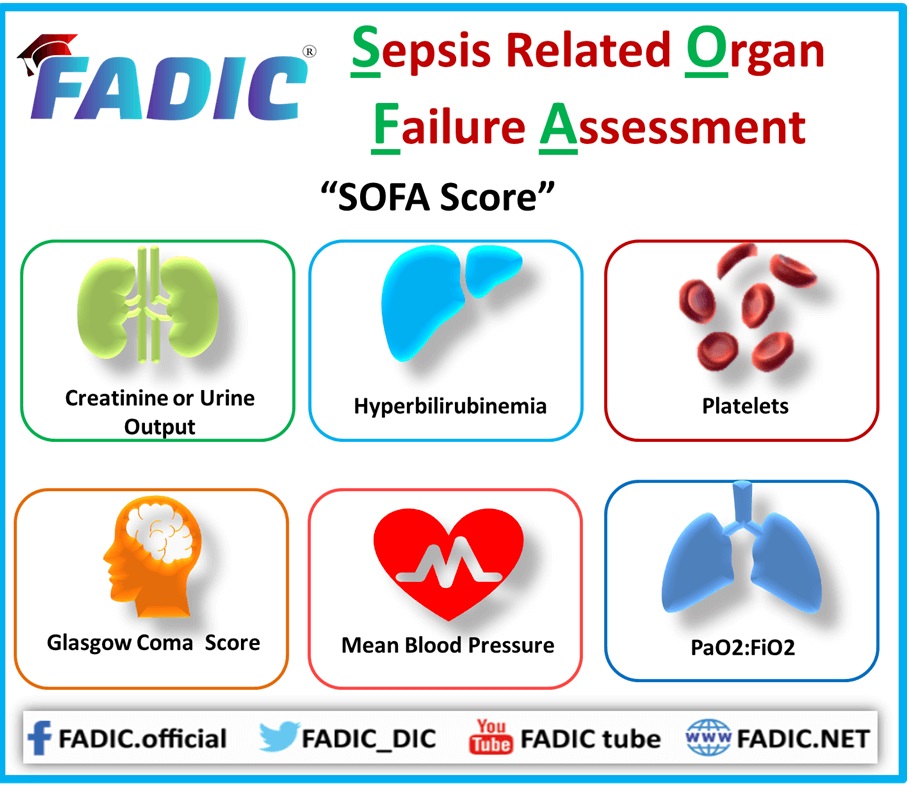
The Sequential Organ Failure Assessment Score
- The Sequential Organ Failure Assessment (SOFA) score was developed using a consensus-based process by an expert committee of the European Society of Intensive Care Medicine in 1994.
- Moreover, tt measures organ dysfunction in the same six systems as the MOD score, using a 5-point scale.
- Its major differences lie in the variable used to describe cardiovascular dysfunction (the dose of vasoactive agents administered), its use of urine output as a descriptor for renal dysfunction, and its use of worst, rather than representative, daily values.
SOFA Score
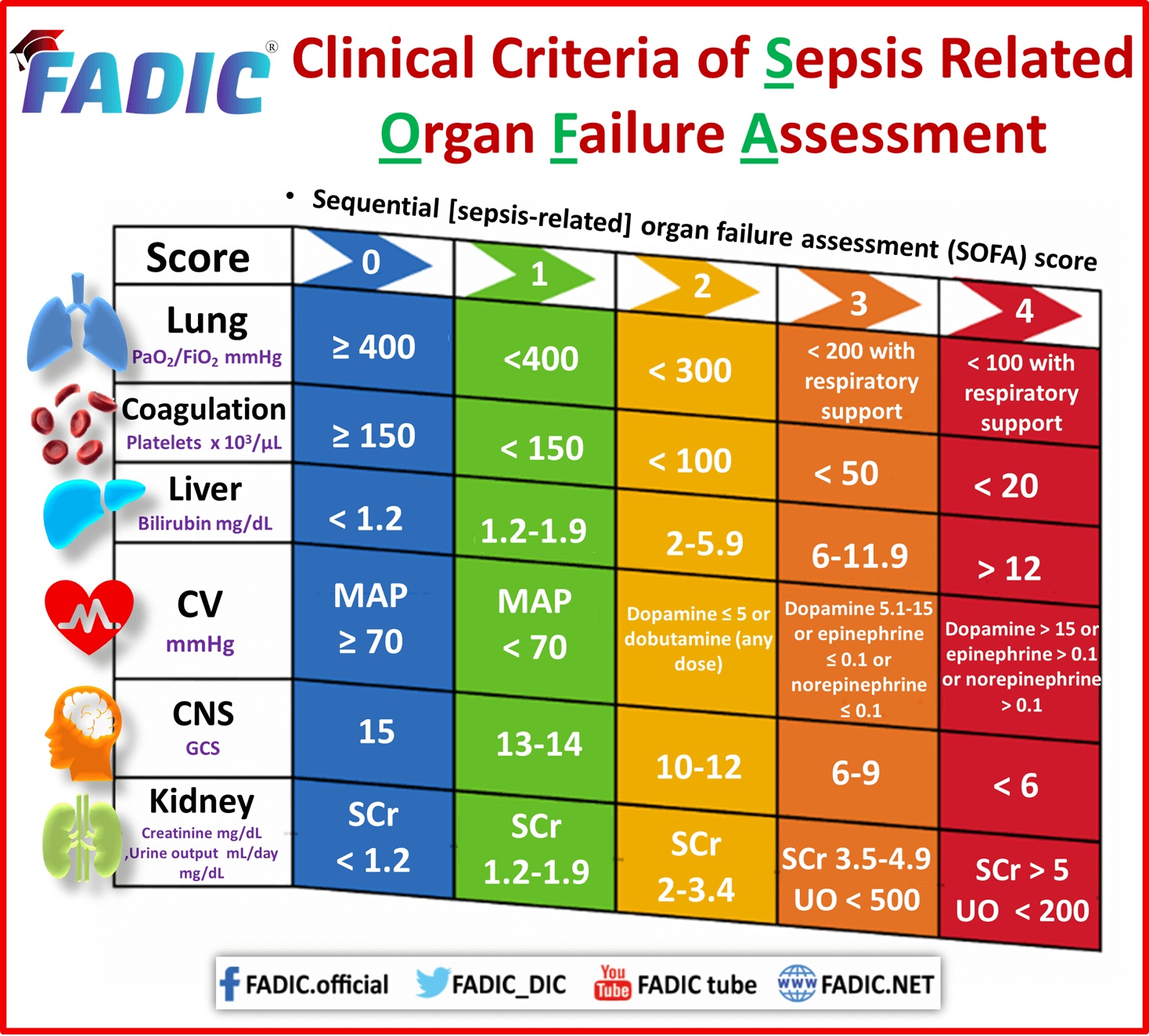
- The SOFA score is based on six different independent scores, including respiratory, cardiovascular, hepatic, renal, coagulation, and neurological systems, and is used to check the patient’s status or the extent of organ failure and dysfunction in intensive care units (ICUs).
- Generally, it is designed to predict the mortality but not the success or failure of medical interventions.
QSOFA
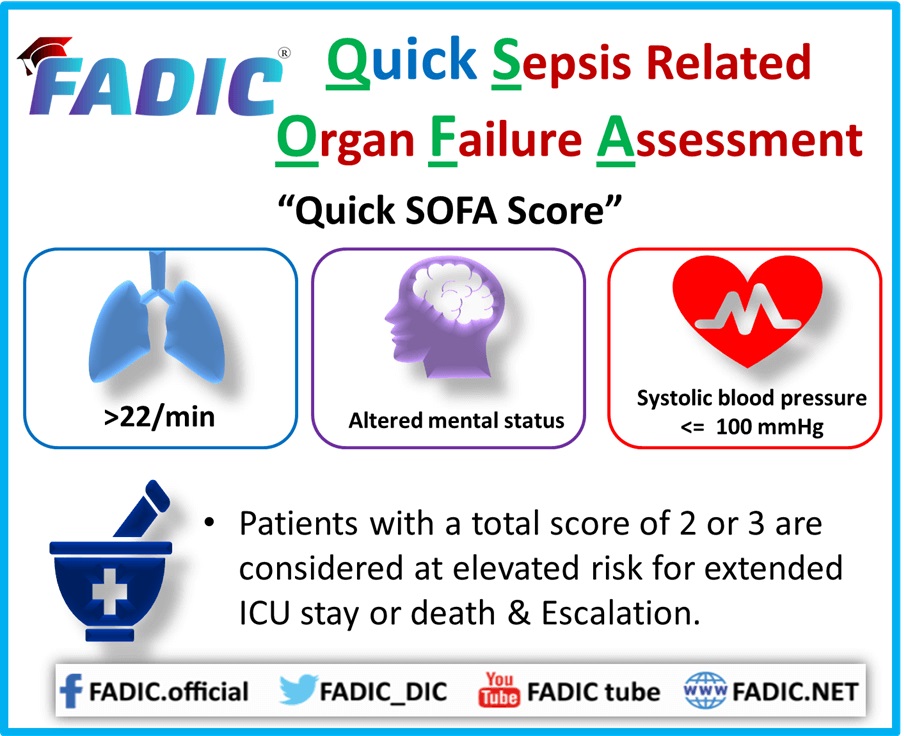
- The concept of quick SOFA (qSOFA) was also introduced by the task force of Sepsis-3, keeping into consideration the limitations of using the SOFA score outside ICUs.
- Therefore, to identify the patients with the highest probability of poor outcome associated with sepsis, a bedside clinical score named as qSOFA was developed, which is based on at least two of the following clinical criteria:
- Respiratory rate of 22 breaths/min or greater
- Systolic blood pressure of 100 mmHg or less
- Altered mentation with Glasgow Coma Scale/Score of 14 or less.
It is a neurological scale for recording a person’s consciousness before and after the assessment
Sepsis Treatment
Goals and principles of treatment in septic shock – The treatment of patients with septic shock has the following major goals:
- Start adequate antibiotic therapy (proper dosage and spectrum) as early as possible
- Identify the source of infection, and treat with antimicrobial therapy, surgery, or both (source control)
- Resuscitate the patient, using supportive measures to correct hypoxia, hypotension, and impaired tissue oxygenation (hypo-perfusion)
- Maintain adequate organ system function by maintaining blood flow and arterial pressure, guided by cardiovascular monitoring, and interrupt the progression to multiple organ dysfunction syndrome (MODS) by appropriate antibiotics and surgical debridement, as needed
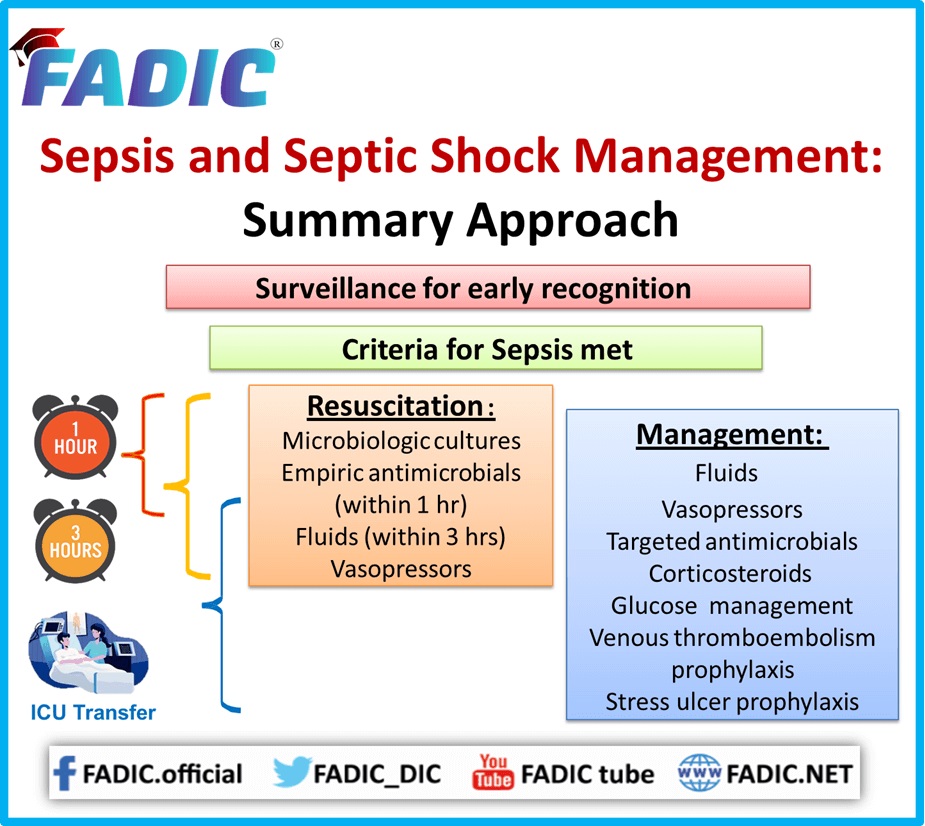
Management principles, based on the current literature, include the following:
- Early recognition
- Source control
- Early and adequate antibiotic therapy
- Early hemodynamic resuscitation and continued support
- Proper ventilator management with low tidal volume in patients with acute respiratory distress syndrome (ARDS)
- Moreover, initial treatment includes support of respiratory and circulatory function, supplemental oxygen, mechanical ventilation, and volume infusion.
- The first 6 hours of resuscitation of a critically ill patient with sepsis or septic shock are critical.
The following should be completed within 3 hours:
- Obtain the lactate level (Although recommended, the three recent trials showed that lactate-guided therapy had no impact on survival. Still, lactate levels parallel septic shock severity and have prognostic implication.)
- Moreover, obtain blood cultures before administering antibiotics
- Administer broad-spectrum antibiotics
- Then, administer 30 mL/kg of crystalloid solution for hypotension or for lactate levels of 4 mmol/L or higher
The following should be completed within 6 hours:
- Administer vasopressors for hypotension that does not respond to initial fluid resuscitation.
- This is to maintain a mean arterial pressure (MAP) of 65 mm Hg or higher.
- The Recent studies showed the validity of the 70-75 mm Hg lower mean arterial pressure target or 80-85 mm Hg in those patients with preexisting hypertension.
- If hypotension persists despite volume resuscitation or the initial lactate level is 4 mmol/L or higher.
- Then measure central venous pressure (CVP) (aiming for ≥8 mm Hg), measure central venous oxygen saturation (ScvO2) (aiming for ≥70%), and normalize lactate levels.
- Finally, the goal of vasopressor therapy is to reverse the pathologic vasodilation and altered blood flow distribution
First-line agents: Norepinephrine vs dopamine
- The recommended first-line agent for septic shock is norepinephrine, preferably administered through a central catheter.
- The dosage range for norepinephrine is 5-20 µg/min, and it is not based on the weight of the patient.
- Norepinephrine is preferred to dopamine for managing septic shock because dopamine is known to cause unfavorable flow distribution (more arrhythmias).
Empiric antimicrobial therapy
- Firstly, initiate early in patients experiencing septic shock (within 1 hour of recognition of septic shock) and sepsis without septic shock, if possible.
- The Surviving Sepsis Campaign guidelines recommend including 1 or more agents that are not only active against the likely organisms but also capable of penetrating “in adequate concentrations into the presumed source of sepsis,”.
- Generally, a 7- to 10-day treatment course is followed.
- Longer treatment regimens warranted in the presence of a slow clinical response, undrainable foci of infection, and immunologic deficiencies (eg, neutropenia).
Combination empiric therapy is recommended for patients with the following:
- Difficult-to-treat, multidrug-resistant microorganisms (eg, Pseudomonas and Acinetobacter species)
- Severe infections associated with respiratory failure and septic shock
- Septic shock and bacteremia from pneumococci
However, combination therapy should be limited to 3-5 days.
After which period treatment should switch to the most appropriate mono-therapy once the results of the susceptibility profile are available.
Antibiotic selection of Antibiotic in Sepsis
(Antimicrobial Stewardship in Sepsis)
- Firstly, the choice of antimicrobial agent can sometimes be daunting. Consideration should be given to the origin (i.e., community- or health care–acquired), site, and source of infection.
- Recently used antibiotics should be avoided if possible, and local susceptibilities should be considered.
- Moreover, the broad-spectrum antibiotics are ideal for empiric therapy, as they provide coverage of multiple organisms.
- Of course, it is important to use clinical judgment, factor in local susceptibilities, and consider the patient’s allergies when initiating empirical antibiotics in any patient.
- Furthermore, treatment of the underlying cause may warrant the use of additional antibiotics.
Monotherapy versus Combination Therapy:- The efficacy of carbapenem monotherapy demonstrated to be equal to the combination of a beta-lactam plus an aminoglycoside.
- Third- or fourth-generation cephalosporin monotherapy shown to be as effective as either a beta-lactam or clindamycin plus an aminoglycoside.
- Additionally, in patients with pneumonia, intra-abdominal infections, or neonatal sepsis, equal efficacy demonstrated for extended-spectrum penicillins with or without a beta-lactamase inhibitor compared with amoxicillin-clavulanate, piperacillin-tazobactam, or clindamycin in combination with an aminoglycoside.
- In general, beta-lactam antibiotics shown to be as efficacious as combination therapy with beta-lactams and aminoglycosides, with fewer renal complications.
- Finally, many recommend combination therapy in neutropenic patients and when certain bacteria suspected, such as Pseudomonas Aeruginosa.
MRSA:
- Underestanding the Microbiology will have great impact in dealing with MRSA.
- Empiric coverage of MRSA is important, as higher mortality rates have been associated with inappropriate antibiotic therapy.
- Vancomycin often utilised as empiric therapy for suspected MRSA infections.
- It is important to ensure that the minimum inhibitory concentration is ≤1 mcg/mL upon receipt of cultures.
- If not, alternative MRSA-susceptible antibiotic therapies (e.g., linezolid, tigecycline, ceftaroline, or daptomycin) should be considered.
Sites of Infection
Lung:
- If the site of suspected infection is the lung, the origin of the infection must be considered.
- Moreover, if the infection is community-acquired, likely pathogens include Streptococcus pneumoniae, Haemophilus Influenzae, Legionella species, and Mycoplasma pneumoniae.
- Respiratory fluoroquinolone as monotherapy or a macrolide antimicrobial, in addition to a beta-lactam (such as a third- or fourth-generation cephalosporin), are good empiric options for community-acquired respiratory infections.
- Moreover, health care–acquired or –associated infections are often caused by Pseudomonas species, MRSA, Klebsiella species, and anaerobic bacteria.
- These infections empirically treated with the combination of a carbapenem or piperacillin-tazobactam, in addition to levofloxacin or ciprofloxacin, plus vancomycin.
IV Catheter–Related Bloodstream Infections:
- Common bacteria associated with IV catheter–related infections include Staphylococcus epidermidis, S aureus, aerobic gram-negative bacilli, and Candida species.
- Vancomycin plus piperacillin-tazobactam is one option for empiric therapy.
- If Candida suspected, antifungal therapy should be considered.
Urinary Tract:
- Urinary pathogens include aerobic gram-negative bacilli, such as E coli, Proteus species, Pseudomonas species, and Enterococcus species.
- For community-acquired urinary infections, empiric treatment with ciprofloxacin or levofloxacin is a good choice, as is treatment with amoxicillin-clavulanate.
- Moreover, resistance to fluoroquinolones is increasing in some regions, so attention paid to local susceptibilities in these instances.
- For urinary infections that are health care–acquired or –associated, empiric treatment with ciprofloxacin or levofloxacin considered, as might treatment with piperacillin-tazobactam or cefepime.
- Pathogens to empirically cover for health care–acquired or –associated infections include Pseudomonas species, MRSA, Klebsiella species, and anaerobes.
- If MRSA suspected, vancomycin added to the empiric regimen.
- Finally, treatment with carbapenem also appropriate; however, caution used in areas with high rates of extended-spectrum beta-lactamase–producing Enterobacteriaceae.
Abdomen:
- Aerobic gram-negative bacilli, anaerobes, and commonly Candida species associated with intra-abdominal infections.
- Moreover, these infections empirically treated with a carbapenem or piperacillin-tazobactam with or without an aminoglycoside.
- Then, antifungal therapy considered.
- For suspected B fragilis or other bacteria that resistant to penicillins, the use of a carbapenem, metronidazole, or a combination penicillin and beta-lactamase inhibitor considered.
Unclear Source
- If the source of infection is unknown or difficult to determine, empiric treatment options include carbapenems plus vancomycin.
- These drugs cover a wide array of bacteria, including aerobic gram-negative bacilli, S aureus, and streptococci.
The Pharmacist’s Role in Sepsis
- Optimally, the pharmacists placed to interact with many different health care professionals, affording them many opportunities to improve patient care via the optimization of sepsis management.
- Implement Antimicrobial Stewardship strategies in Sepsis
- Among these opportunities are appropriate antibiotic selection, de-escalation of antibiotic therapy, and sepsis bundle (protocol) implementation.
Selection of Appropriate Antibiotic:
- Selection of broad-spectrum antibiotics should be targeted toward likely pathogens.
- Pharmacist should learn all about the antimicrobials
- A simple way to accomplish this is to review the admission diagnosis when entering orders for antibiotics to verify the indication for antibiotic choice.
- Moreover, the pharmacist can also examine reasons for a change in antimicrobial therapy.
De-escalation of Antibiotic Therapy
- Antibiotic stewardship requires de-escalation of the antibiotic regimen when necessary.
- This serves to prevent the unwanted effects of broad-spectrum antibiotic overuse, such as increased resistance, cost, and adverse events.
- Once cultures have been obtained and results available, review the antibiotic therapy to ascertain that the pathogen is susceptible to the prescribed drug regimen.
- In addition, consideration given to utilising a more limited spectrum antibiotic shows efficacy.
Sepsis Bundle (Protocol) Implementation
- Clinical evidence shows that the treatment of sepsis with evidence-based protocols, or bundles, improves treatment outcomes.
- Sepsis bundles based on the Surviving Sepsis Campaign combine individual interventions or orders with the goal of improving outcomes.
- These bundles place labs and medications on one order form to ensure that nothing accidentally omitted.
- Unfortunately, the implementation of clinical evidence into practice can present many difficulties, including provider acceptance, a perception of “cookbook medicine,” and the approval process.
- As patient advocates, pharmacists uniquely positioned to champion acceptance and implementation of such bundles, as many of the interventions are medication-related.
- Education of all involved professionals is key to the buy-in, proper implementation, and success of sepsis bundles.
- Of course, outcomes must continually assessed to determine the effectiveness of the sepsis bundle.
Sepsis Prevention
Patients with impaired host defense mechanisms are at greatly increased risk for sepsis.
The main causes of impaired host defense are as follows:
- Chemotherapeutic drugs
- Malignancy
- Severe trauma
- Burns
- Diabetes mellitus
- Renal or hepatic failure
- Advanced age
- Ventilatory support and invasive catheters further increase the risk of infection.
- Avoiding the use of catheters or removing them as soon as possible may prevent sepsis.
- Prophylactic antibiotics in the preoperative phase, particularly after GI surgery, may be beneficial.
- The use of topical antibiotics around invasive catheters and as part of dressings for patients with burns is helpful.
- Other preventive measures include maintenance of adequate nutrition, administration of pneumococcal vaccine in patients who have undergone splenectomy, and early enteral feeding.
- Prevention of sepsis with topical or systemic antibiotics suggested for high-risk patients.
- Finally, use of non-absorbable antibiotics in the stomach to prevent translocation of bacteria and occurrence of bacteremia is a controversial issue.
Basic measures to prevent nosocomial infections include the following:
- Shortening the hospital stay
- Removing indwelling catheters as early as possible
- Avoiding unnecessary invasive procedures
- Using aseptic techniques
Conclusion:
- Sepsis is the body’s extreme response to an infection, it is a life-threatening medical emergency.
- Without timely treatment, sepsis can rapidly lead to tissue damage, organ failure, and death.
- It is important to update yourself with every news especially in the Infectious Disease, as here in E-News (Free Subscribed)
Read More:
- Antimicrobial Stewardship School
- Sepsis Training Program
- Download Pocket Guide for Antibiotic Pharmacotherapy Book
- Microbiology Course | ABC Bacteria
- Infectious Disease E-News | FREE Subscription
- ABC antimicrobials | Know all about the Antimicrobials
- Road Map to Antimicrobial Stewardship Training Program
- Register Now in FADIC Clinical Research School
- FADIC Drug Information Fellowship
- Buy FADIC Toolkit for Writing Research to Write a Great Research Paper
- Read 10 Skills You Must Learn to Make a Research via Google Scholar in Arabic
- The FADIC Online Continuous Medical Improvement Programs & Mini-Courses.
- Check Now FADIC Book store and Buy books in different specialties.
- Watch Now FADIC TV to Keep your self Updated.
- FADIC Podcast focusing on varieties of pharmacist perspectives in different specialties.
- Subscribe Now in FADIC 2020 Daily News (FNN) and Keep Updated.
- Check Now about Coronavirus Resource Information Center.

 Log in
Log in Sign up
Sign up