Six Bacteria Cause the Antimicrobial Resistance
Six Bacteria Cause the Antimicrobial Resistance
The Six Pathogens Cause This Global Burden
- Escherichia coli
- Staphylococcus aureus
- Klebsiella pneumonia
- Streptococcus pneumonia
- Acinetobacter baumannii
- Pseudomonas aeruginosa
- Antimicrobial resistance (AMR) is one of the most severe global health burdens.
- Six Bacteria Cause the Antimicrobial Resistance.
- This burden is responsible for millions of deaths globally per year.
- Moreover, it was declared by the world health organisation (WHO) as the most severe threat facing humanity.
- Antimicrobial-bacterial resistance is the ability of bacteria to become unresponsive to antibiotic treatment.
- The overuse and misuse of antibiotics cause this global crisis. Six pathogens were reported as causing mortality associated with resistance.
- A high-level resistance in successive bacterial generations generates hypermutable bacterial strains (increase the mutation rate)
- Moreover, it may increase the ability to acquire resistance to other antimicrobial agents.
- Escalating the use of antimicrobials in animals and agriculture is increasing the problem of drug resistance.
- A high level of resistance to several bacterial severe infections has been reported globally.
- Additionally, the Food and Drug Administration (FDA) and the Centers for Disease Control and Prevention (CDC) reported that the key to controlling the spread of resistance is to raise awareness about this burden and avoid the overuse of antibiotics.
Highly recommend online Marketing tool from SEMRUSH
What is the Misuse of antibiotics?
- Overuse of antibiotics.
- Low or sub-dosing with antibiotics or not completing the treatment course.
- Using antibiotics for treating viral infections.
- Additionally, using antibiotics in farming (resistant bacterial strains can spread to humans from food and animals).
What are the types of resistance?
Antimicrobial resistance can be divided into intrinsic or inherent resistance and acquired resistance:
- Intrinsic resistance: a resistance results from a bacteria’s genetic, structural, or physiological characteristics.
- Additionally, acquired resistance: a resistance that results from altered cellular physiology and structure caused by a change in a microorganism’s usual genetic makeup.
What is the Mechanism of antimicrobial resistance?
- Antibiotics kill harmful bacteria; some bacteria may survive (resistant bacteria). These resistant bacteria multiply and pass on their resistant gene.
- Additionally, a new population of bacteria with drug resistance traits is spread.
Antimicrobial resistance mechanisms include:
1-Limiting drug uptake.
- The ability of bacteria to limit the uptake of antimicrobial agents differs according to the structure of the cell wall.
- Additionally, the lipopolysaccharide layer in gram-negative bacteria provides a barrier to a specific type of molecules.
- Moreover offers gram-negative bacteria an innate resistance to several antimicrobial agents.
- A strain of staphylococcus aureus bacteria developed an intermediate resistance to vancomycin.
- Lastly, this strain of Staphylococcus aureus produced a thickened cell wall which limited the entry of the drug (vancomycin) into the cell.
2- Modifying a drug target.
- Modifying bacterial cell components that antimicrobial agents target.
- Gram-positive bacteria’s resistance mechanism to the β-lactam drugs is via alterations in the number and structure of penicillin-binding proteins.
- Interestingly, A change in the design of penicillin-binding proteins in Staphylococcus aureus inhibits drug binding.
- Moreover, the changes in the form of peptidoglycan precursors in vancomycin resistance Staphylococcus aureus cause a decrease in the binding ability of vancomycin.
- In conclusion, another drug resistance mechanism is fluoroquinolones resistance which is a drug that targets nucleic acid synthesis.
- Additionally, this resistance is due to the modifications in DNA gyrase in gram-negative bacteria or topoisomerase IV in gram-positive bacteria.
- Interestingly, these mutations cause changes in the structure of gyrase and topoisomerase, limiting the drug’s ability to bind to these components.
- Lastly, mutations in some bacterial enzymes may inhibit some antimicrobial drugs that target specific bacterial enzymes.
3- Drug inactivation.
- Drug inactivation either by degradation of the drug or by transfer of a chemical group to the drug.
- Additionally, the most widely used antimicrobial agents are β-lactam drugs. Resistance to the β-lactam drugs occurs through hydrolysis of the drug by β-lactamase enzymes and alterations in the number and structure of penicillin-binding proteins.
- Moreover, staphylococcus aureus, Streptococcus pneumonia, and Klebsiella pneumonia are resistant to β-lactam drugs.
4- Active drug efflux.
- Some bacteria are resistant due to efflux pumps genes expressed upon stress or acquired upon mutation.
- These pumps allow the bacteria to get rid of toxic substances by transporting a large variety of poisonous compounds outside of bacterial cells.
- Bacteria possess genes encoded for efflux pumps. Some bacteria express a high-level resistance via a mutation that modifies the transport channel.
- Moreover, certain bacteria possess efflux pumps that can extrude β-lactam drugs. Drug-resistant bacteria that may use drug efflux mechanisms include Escherichia coli, Staphylococcus aureus, Acinetobacter baumannii, and Pseudomonas aeruginosa.
- Importantly, Resistant mechanisms differ among types of bacteria. Intrinsic resistance uses drug inactivation, limiting uptake, and drug efflux. Acquired resistance mechanisms include drug target modification, drug inactivation, and drug efflux.
- Additionally, the mechanisms used differ according to the bacterium’s structure. Gram-negative bacteria use all four main instruments. Gram-positive bacteria use the tool of limiting the uptake of a drug as it does not have lipopolysaccharides in the outer membrane and does not have the capacity for specific types of drug efflux mechanisms.
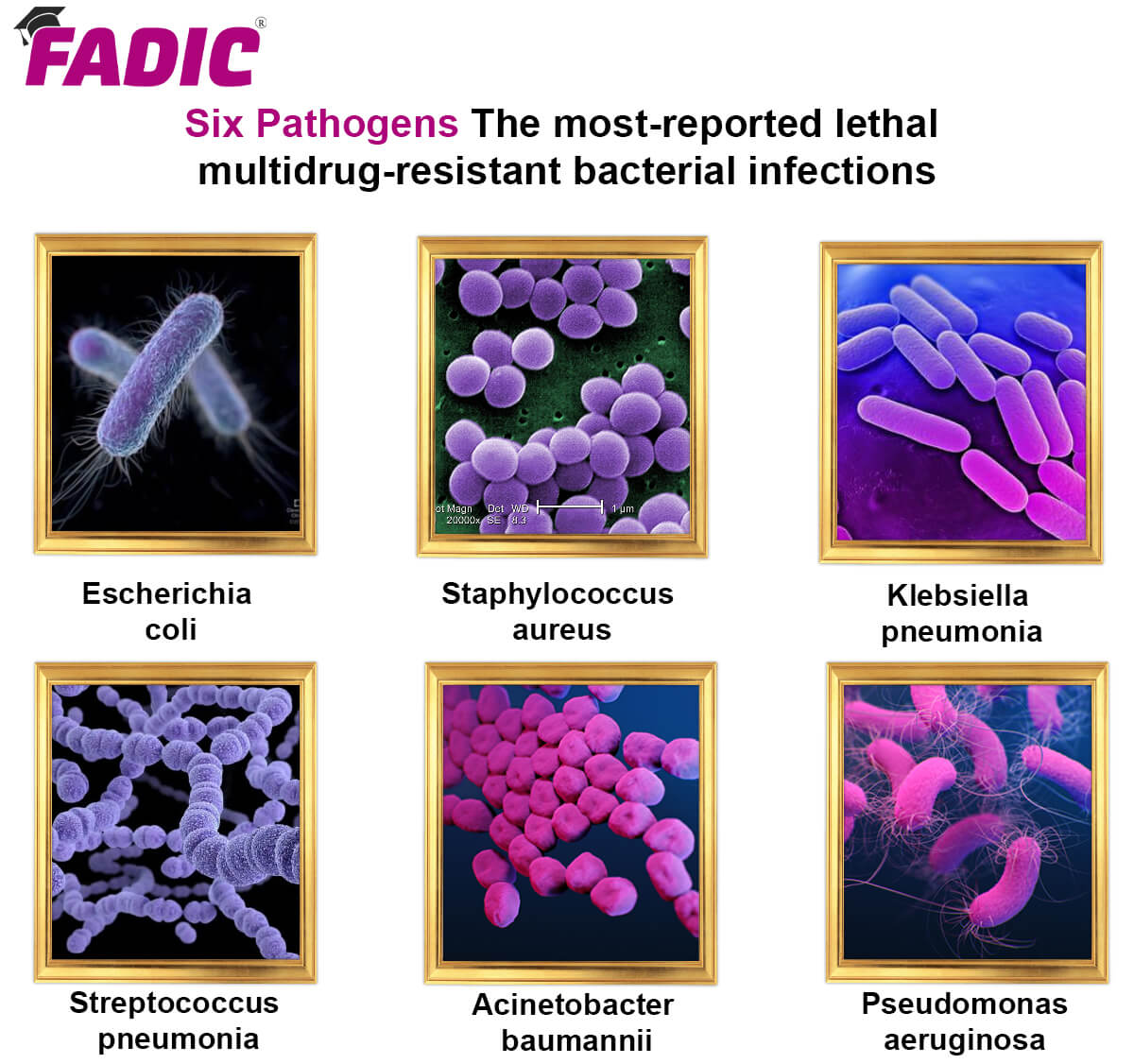
The most-reported lethal multidrug-resistant bacterial infections were:
1- Escherichia coli
2- Staphylococcus aureus
3- Klebsiella pneumonia
4- Streptococcus pneumonia
5- Acinetobacter baumannii
6- Pseudomonas aeruginosa
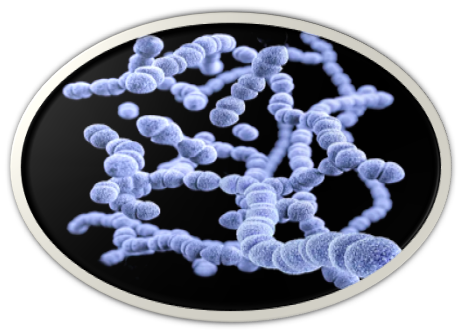
Escherichia coli

Overview
- Escherichia coli (E. coli) is one of The ix Bacteria that Cause Antimicrobial Resistance.
- It is a Gram-negative, facultatively anaerobic, and rod-shaped bacterium. Coli is a diverse group of bacteria and ordinary residents of the healthy people’s gut.
- Moreover, most strains of E. coli are harmless, while certain strains of the bacterium are reported to be responsible for infant diarrhoea and gastroenteritis. Several songs of E-coli are present. The most common themes for severe infections outbreak include:
- Shiga toxin-producing E. coli (STEC): This strain is responsible for foodborne illness.
- Enterotoxigenic E. coli (ETEC): This strain is responsible for traveller’s diarrhoea.
- The Shiga toxin-producing E. coli (STEC) causes bloody diarrhoea, severe kidney failure, and death.
- Additionally, the infection can occur in people of all ages and is most common in children and adults with weak immune systems. E-coli strain shows resistance to fluoroquinolone antibiotics.
Symptoms of infection
- Shiga toxin-producing E. coli (STEC) causes severe foodborne disease. Signs of illness occur within 24 hours; it takes about 3 to 4 days or even lasts ten days. STEC infection is associated with a severe complication called hemolytic uremic syndrome, leading to kidney failure and death.
Symptoms include:
- Fever
- Nausea
- Vomiting
- Severe abdominal cramps
- Watery or very bloody diarrhoea
- Constant fatigue
Sources and transmission
- Shiga toxin-producing E. coli (STEC) causes severe foodborne disease.
- Additionally, it is usually transmitted to people when they eat foods contaminated with bacteria.
- Moreover, the infection also can occur by swallowing swimming pool water contaminated with human waste.
- Importantly, patients in intensive care units may acquire this bacterium from ventilators.
- Lastly, severe food-borne diseases can be prevented by handling food safely. Eat well-cooked meat, wash fruits and vegetables before eating or cooking them, and avoid unpasteurised milk and juices.
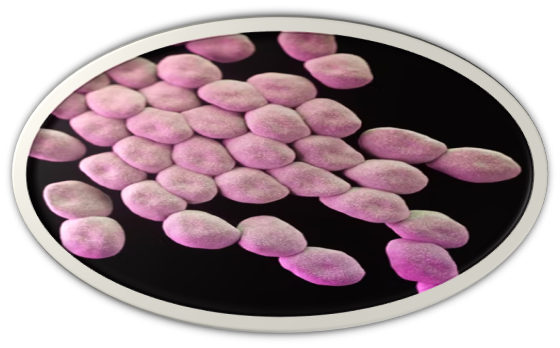
Staphylococcus aureus
Overview
- Staphylococcus aureus is anaerobic and is one of the Six Bacteria Cause Antimicrobial Resistance.
- It is gram-positive cocci are part of the normal skin and upper respiratory tract flora.
- This bacterium is both a commensal bacterium and a human pathogen.
- Staphylococcus aureus infections include food poisoning, endocarditis, toxic shock syndrome, and pneumonia.
- It also causes bloodstream infections, bone-joint infections, and skin and soft tissue infections.
- Staphylococcus aureus infections are common both in community-acquired and hospital-acquired settings.
- Treatment remains challenging due to the emergence of multi-drug resistant strains such as MRSA (Methicillin-Resistant Staphylococcus aureus).
- Moreover, these bacterium expresses several virulence factors and harbours antibiotic resistance genes.
- Many staph antibiotic-resistant strains were observed, which include:
- Methicillin-resistant Staphylococcus aureus (MRSA): Multidrug-resistant strain to a class of antibiotics called beta-lactams.
- Additionally, this group of antibiotics includes methicillin, penicillin, amoxicillin, and oxacillin.
- Methicillin-sensitive Staphylococcus aureus (MSSA): staph strain sensitive to methicillin and less virulent than MRSA. It is susceptible to antibiotics.
- Community-acquired MRSA (CA-MRSA): staph strain that occurs outside hospital settings and usually manifests as a skin infection. It can lead to a more serious life-threatening illness.
- Vancomycin-intermediate Staphylococcus aureus (VISA): staph strain that exhibits intermediate resistance levels.
- Vancomycin-resistant Staphylococcus aureus (VRSA): staph strain resistant to vancomycin therapy, rare but seen on long-term vancomycin therapy.
The symptoms
- The symptoms of a staph infection depend on the strains and site of infection.
- Additionally, Staph skin infections are the most common.
- Moreover, these bacteria cause invasive infections and toxin-mediated diseases.
Symptoms of a staph skin infection include:
- Abscesses and boils: The most common type of infection is a pocket of pus that develops in a hair follicle or oil gland that is painful and red sores. It usually grows under the arms, inner thighs, and buttocks.
- Cellulitis: an infection of the deeper layers of skin that appears as swollen, hot red, and painful skin.
- Impetigo: painful small blisters filled with fluid that may rupture, leaving a yellow or yellow-brown crust which is contagious.
- Folliculitis: A small pimple-like blister forms under the hair follicle and causes pain.
- Staphylococcal scalded skin syndrome: This severe infection is caused by staph bacteria toxin. It usually affects infants and children. Blisters that break cause the top layer of skin to peel. This leaves a red surface that looks like a burn and is very painful.
The symptoms of invasive staph infections include:
- Staph food poisoning: Symptoms include severe vomiting, diarrhoea, and abdominal cramps.
- Septicemia or sepsis: Staph infection of the bloodstream can cause blood poisoning, which leads to a widespread inflammatory response.
- The symptoms include fever and severe hypotension. A life-threatening condition can spread throughout the body, affecting the function of internal organs.
- Toxic shock syndrome: A severe form of septicemia, this serious condition can happen when staph bacteria enter the bloodstream and produce toxins.
- Additionally, the symptoms include fever and a rash that looks like sunburn.
- Endocarditis: staph infection of the lining of the heart muscle. If not treated quickly, it is a severe condition; heart valves and muscles may be damaged.
- Therefore, the symptoms include fever and fast heart rate.
- Pneumonia: An acute inflammation of lung parenchyma where alveolar damage and fluid accumulation in the lungs may occur.
Sources and transmission
- Staph food poisoning occurs by eating foods contaminated by staph toxins. Foods typically become contaminated due to handling by staph-infected people. Staph skin infection can occur in individuals sharing personal items such as towels.
- Additionally, Close contact between children in childcare and soldiers and prisoners in long-term care facilities increases the risk of infection. Contaminated medical equipment such as invasive techniques. Generally, staph is spread by contact with contaminated items or environmental surfaces.
Klebsiella pneumonia
Overview
- Klebsiella pneumoniae is a member of Enterobacteriaceae. It also is one of Sthe ix Bacteria Cause Antimicrobial Resistance.
- The Klebsiella is a type of gram-negative bacteria, encapsulate, and non-motile bacterium that belongs to the normal flora of the human oral cavity and intestine.
- These intestinal bacteria are harmless, but if they spread to another part of the body.
- Additionally, they can cause severe infections.
- K. pneumonia usually affects patients with an impaired immune system and tends to become antibiotic-resistant.
- The pathogenic Klebsiella species, K. pneumonia, is a significant cause of hospital-acquired infections such as pneumonia, bacteremia, wound or surgical site infections, and meningitis in newborns and intensive-care unit patients.
- pneumonia has become highly resistant to antibiotics, most recently to a class of antibiotics known as carbapenems. Carbapenem antibiotics are the last defence against gram-negative infections resistant to other antibiotics.
- K. pneumonia is highly resistant to carbapenem antibiotics due to producing carbapenemase enzyme.
- Additionally, in some cases reported, Klebsiella shows resistance to colistin antibiotics, the last line of defence against carbapenem-resistant strains.
The symptoms
- Bacteria enter the host following oropharyngeal aspiration causing pneumonia
symptoms of pneumonia include:
- Fever
- Shortness of breath
- Chest pain
- Coughing yellow or bloody mucus
- Klebsiella is reported to cause sepsis and meningitis from a lung infection.
- Moreover, k. pneumonia also can cause urinary tract infections; patients may experience the following symptoms: Fever – Nausea and vomiting – Back pain – Painful or bloody urination
Sources and transmission
- Klebsiella pneumonia accounts for approximately 11.8% of all hospital-acquired pneumonia worldwide.
- Additionally, it spreads through person-to-person contact (from patient to patient via the contaminated hands of healthcare personnel, from ventilators and invasive devices; catheters). Personal hygiene and sanitation of medical equipment can help control the spread.
Streptococcus pneumonia
Overview
- Streptococcus pneumoniae is one of the Six Bacteria Cause Antimicrobial Resistance.
- And it is a gram-positive, facultatively anaerobic, lancet-shaped bacterium commonly found in the upper respiratory tract.
- pneumonia is the most common cause of community-acquired pneumonia (CAP), acute sinusitis, acute otitis media, chronic bronchitis, and more invasive infections, such as meningitis and bacteremia. Also, it may cause endocarditis, septic arthritis, and osteomyelitis.
- pneumonia affects children, immunocompromised individuals, people with severe medical conditions, and the elderly.
- Moreover, this globally infectious pathogen has developed increased resistance to multiple classes of antibiotics such as Beta-lactams (penicillins, cephalosporins, and carbapenems), Macrolides (erythromycin, azithromycin, clarithromycin), and Lincosamides (clindamycin).
The symptoms
- Streptococcus pneumonia can lead to local or systemic infections by spreading from the nasopharynx.
- Sadly, it can lead to local conditions such as sinusitis or acute otitis media and can directly apply to the lungs.
- Additionally, it leads to pneumonia with pleural empyema.
- The symptoms vary according to the infection site.
- Additionally, the symptoms of streptococcus pneumonia infection include an abrupt onset of fever and chills.
Other symptoms may include:
- Headache
- Cough
- Chest pain and shortness of breath
- Weakness
- Disorientation
- Increased sensitivity to light
- Joint pain
- Ear pain
Moreover, pneumococcal disease can cause loss of hearing, brain damage, and death.
Sources and transmission
- Streptococcus Pneumococcal infections are most prevalent during the winter and early spring.
- Infection is spread from person to person by inhaling or direct exposure to the droplets through coughing or sneezing an infected person.
- Additionally, A pneumococcal vaccine is now available to help reduce the widespread pneumococcal infection.
Acinetobacter baumannii
Overview
- Acinetobacter baumannii is one of the Six Bacteria Cause Antimicrobial Resistance.
- Also, it is a gram-negative, aerobic bacillus and non-motile bacterium.
- This bacterium is the most important pathogen associated with hospital-acquired infections worldwide.
- A. baumannii has a high incidence among immunocompromised individuals and elders.
- It resists many classes of antibiotics due to its relatively impermeable outer membrane and chromosome-mediated genetic features.
- These features allow it to survive for a prolonged period in harsh environments and hospital settings.
- Additionally, A. baumannii infection includes bacteremia, pneumonia, meningitis, urinary tract infection, and wound infection.
The symptoms
- baumannii is a nosocomial pathogen.
- The symptoms may vary but can also be asymptomatic.
- A. baumannii infections are very variable and include soft tissue, skin, wound infections, urinary tract infections, and pneumonia.
- It also may cause gastrointestinal tract infections and eye infections, including keratitis and endophthalmitis, osteomyelitis, meningitis, and endocarditis.
- Moreover, A. baumannii infections can be complicated by extensive soft tissue necrosis, sepsis, acute respiratory distress syndrome, multi-organ failure, and death.
- Additionally, the symptoms vary for each type of infection.
Sources and transmission
- Baumannii is highly contagious. The infection is transmitted through direct and indirect contact (hands, medical materials, or instruments) and contaminated water or food.
- Acinetobacter can live for long periods on environmental surfaces and used equipment if they are not adequately cleaned.
- Moreover, acinetobacter infection outbreak usually occurs in hospital intensive care units and healthcare settings.
- Additionally, applying hygienic measures can help control the spread of infection.
Pseudomonas aeruginosa
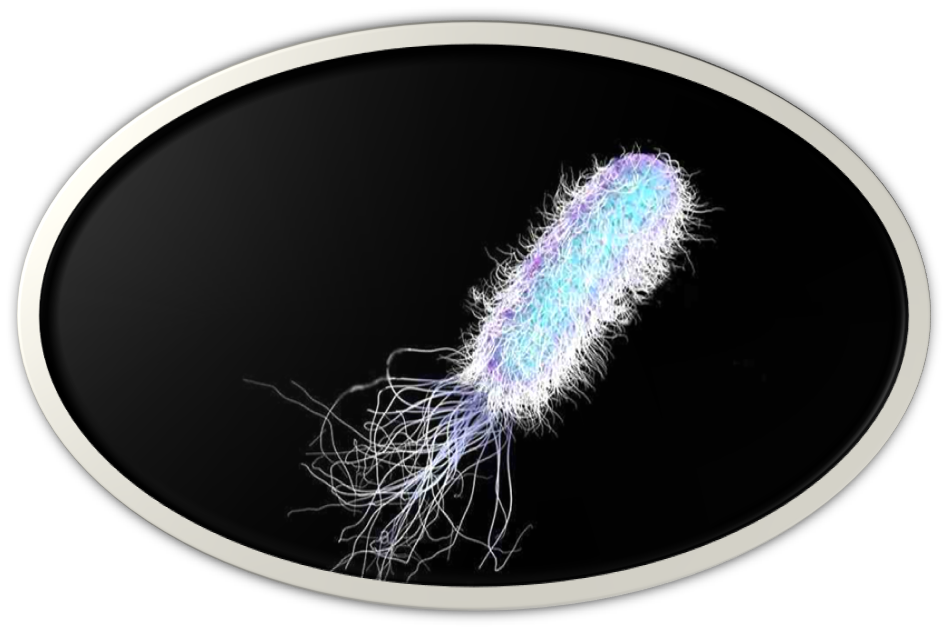
Overview
- Pseudomonas aeruginosa is one of the Six Bacteria CthatChat cause Antimicrobial Resistance.
- Also, it is a gram-negative, aerobic, non-spore-forming rod that can cause several life-threatening acute and chronic infections, particularly in immunocompromised patients.
- This pathogen is one of the leading nosocomial pathogens affecting hospitalised patients intrinsically multidrug-resistant.
- Pseudomonas aeruginosa infection includes many community-acquired disorders like folliculitis, osteomyelitis, endocarditis, pneumonia, and otitis infection.
The symptoms
The symptoms of Pseudomonas aeruginosa infection may vary and include:
- Otitis infection: pain and discharge.
- Pneumonia: severe coughing and difficulty of breathing.
- Eye infection: pain, redness, and swelling.
- Skin infection: rash, pain, and folliculitis.
- Bones or joint infection: joint pain and swelling.
- Urinary tract infections: painful urination and may be bloody.
- Digestive tract infection: headache, vomiting, and diarrhoea.
Sources and transmission
- Pseudomonas aeruginosa lives in the environment, particularly in soil and water contaminated with these bacteria.
- Reservoirs may contain this Pseudomonas aeruginosa, including icemakers, jacuzzis, and swimming pools.
- Resistant strains spread from one person to another through contaminated hands, medical equipment, and surfaces.
- Infections with this pathogen may include ventilator-associated pneumonia and catheter-associated urinary tract infections.
Conclusion
- Firstly, antimicrobial resistance (AMR) to several commonly used antibiotics is wide-spreading globally.
- Secondly, drug resistance adaptations are accelerated by the overuse and inappropriate use of antibiotics.
- Thirdly, and most importantly, it is essential to monitor the antimicrobial resistance patterns periodically,
- Moreover, formulations of new classes of drugs, combined antibiotic therapy under prescription and spread awareness of safe antibiotic usage.
- In conclusion, these are the Six Bacteria that Cause the Antimicrobial Resistance
Read More
- Learn more about Antimicrobial Stewardship Program in Acute-care Settings
- Quick Guide for Antimicrobial Stewardship Program
- Download Infectious Disease Pharmacotherapy E-Book
- Join FADIC Clinical Microbiology Mini-course and MDRs
- Subscribe FREE to Antimicrobial Resistance FNN Daily E-News
- Read the lancet study of the six pathogens that cause global antimicrobial resistance burden
 Log in
Log in Sign up
Sign up