Types of Headaches
 Types of Headaches
Types of Headaches
Types of common headaches
Many of us are familiar with some form of a headache’s throbbing, uncomfortable, and distracting pain.
There are different types of headaches.
The common types of headaches include:
- Allergy or sinus headache
- Hormone headache
- Caffeine headache
- Exertion headache
- Hypertension headache
- Rebound headache
- Post-traumatic headache
- Spinal headache
- Tension headache
- Cluster headache
More Types:
- migraine headache
- hemicrania continua
- ice pick headache
- thunderclap headache
Nearly everyone experiences a headache occasionally. The cause, duration, and intensity of this pain can vary according to the type of headache.
If your headache is less severe, read on to learn how to identify the type of headache you may be experiencing and what you can do to ease your symptoms. These are the Types of Headaches

The most common primary headaches
Primary headaches occur when the pain in your head is the condition. In other words, your headache is not triggered by something your body is dealing with, like illness or allergies.
These headaches can be episodic or chronic:
- Episodic headaches may occur every so often but no more than 15 days in one month. They can last anywhere from half an hour to several hours.
- Chronic headaches are more consistent. They occur more than 15 days a month. In these cases, a pain management plan is necessary.
The most common secondary headaches
- Secondary headaches are a symptom of something else that is going on in your body. If your secondary headache triggers are ongoing, your headaches can become chronic. Treating the primary cause generally brings headache relief.
Highly recommend the online Marketing tool from SEMRUSH.
Allergy or sinus headache
- Headaches sometimes happen as a result of an allergic reaction. The pain from these headaches is often focused in your sinus area and the front of your head.
- Migraine headaches are commonly misdiagnosed as sinus headaches. According to the American Migraine Foundation, up to 90 per cent of “sinus headaches” are migraines. People with chronic seasonal allergies or sinusitis are susceptible to these headaches.
Hormone headache
- Women commonly experience headaches that are linked to hormonal fluctuations. Menstruation, birth control pills, and pregnancy affect estrogenic levels, which can cause headaches.
- Those headaches associated with the menstrual cycle are also known as menstrual migraines. These can occur right before, during, or after your period and ovulation.
OTC pain relievers like naproxen (Aleve) or prescription medications like frovatriptan (Frova) can work to manage pain.
According to a 2015 study, about 60 per cent of Trusted sources of women with migraine also experiences menstrual migraine, so alternative remedies may have a role in decreasing overall headaches per month. The following may help
- relaxation techniques
- yoga
- acupuncture
- eating a modified diet
- Caffeine headache
Keeping your caffeine intake at a steady, reasonable level — or quitting it entirely — can prevent these headaches.
Caffeine headache
- Caffeine affects blood flow to your brain. Too much can give you headaches, as can quitting caffeine “cold turkey.” People with frequent migraine headaches risk triggering a headache due to caffeine use.
- When you are used to expose your brain to a certain amount of caffeine, a stimulant, each day, you might get a headache if you do not get caffeine. This may be because caffeine changes your brain chemistry, and withdrawal can trigger a headache.
Exertion headache
- Exertion headaches happen quickly after periods of intense physical activity. Weightlifting, running, and sexual intercourse are all common triggers for an exertion headache. It is thought that these activities cause increased blood flow to your skull, which can lead to a throbbing headache on both sides of your head.
- An exertion headache should not last too long. This type of headache usually resolves within a few minutes or several hours.
- OTC pain relievers, such as aspirin or ibuprofen (Advil), typically ease symptoms.
- If you develop exertion headaches often, see a doctor. In some cases, they may indicate a severe underlying condition.
Hypertension headache
- High blood pressure can cause a headache. This kind of headache signals an emergency. It occurs when your blood pressure becomes dangerously high.
- A hypertension headache usually occurs on both sides of your head and is typically worse with any activity. It often has a pulsating quality.
- You are more likely to develop this type of headache if treating high blood pressure.
- These headaches typically go away soon after blood pressure is under better control. They should not reoccur if high blood pressure continues to be managed.
Rebound headache
- Rebound headaches, also known as medication overuse headaches, can feel like a dull, tension-type headache, or they may feel more intensely painful, like a migraine headache.
- You may be more susceptible to this type of headache if you frequently use over-the-counter (OTC) pain relievers. Overuse of these medications leads to more headaches rather than fewer.
- Rebound headaches are likelier to occur anytime OTC medications are used more than 15 days out of a month. These OTC medications include:
- acetaminophen
- ibuprofen
- aspirin
- naproxen
They are also more familiar with medications that contain caffeine.
- The only treatment for rebound headaches is to wean yourself off the medication you have taken to manage pain. Although the pain may initially worsen, it should completely subside within a few days.
- an excellent way to prevent medication overuse headaches is to take a daily preventive medication that does not cause rebound headaches and prevents the headaches from occurring.
Post-traumatic headache
- Post-traumatic headaches can develop after any head injury. These headaches feel like migraine or tension headaches. They usually last up to 6 to 12 months after your injury occurs. They can become chronic.
Doctors often prescribe the following medications to manage these headaches:
- triptans
- sumatriptan (Imitrex)
- beta-blockers
- amitriptyline
- Spinal headache
Initial treatment for spinal headaches usually includes pain relievers and hydration. It also helps to avoid being in an upright position. Symptoms typically go away on their own after a week or two.
In some cases, an epidural blood patch might be used. This is a procedure in which a small amount of blood is taken from your body and injected back into your epidural space. It can help stop cerebrospinal fluid from leaking, eliminating headaches.
Spinal headache
- A spinal headache results from low cerebrospinal fluid pressure following a lumbar puncture. For this reason, it is also known as a postural puncture headache. You might feel this headache in your:
- forehead
- temples
- upper neck
- back of the head
- Research estimates that spinal headaches follow a lumbar puncture between 10 and 40 per cent Trusted Source of the time. Onset usually begins within 2 to 3 days but could start several months later.
- Other symptoms of spinal headache include:
- nausea
- neck pain
- dizziness
- visual changes
- tinnitus
- hearing loss
- radiating pain in the arms
When to see a doctor
- In most cases, episodic headaches will go away within 48 hours. If you have a headache that lasts more than two days or increases in intensity, see a doctor for help.
- If you are getting headaches more than 15 days out of the month over three months, you might have a chronic headache condition. Even if you can manage the pain with OTC medications, see a doctor for a diagnosis.
- Headaches can be a symptom of more severe health conditions, and some require treatment beyond OTC medications and home remedies.
Diagnosing headaches
- Because there are many types of headaches, many methods might be used to diagnose which type of headache you are experiencing. To receive adequate treatment, it is essential to determine whether you have a primary or secondary headache.
- You can expect your headache diagnosis to begin with a physical exam and a thorough medical history. If possible, keep a “headache journal” in the weeks leading up to your doctor’s appointment. Document each of your headaches, including:
- duration
- intensity
- location
- possible triggers
- Your primary care doctor might also refer you to a specialist, such as a neurologist. You could require diagnostic tests to determine the underlying cause for some headache types. These tests can include:
- MRI or CT scan
- lumbar puncture
- blood tests
- Management and treatment
- Different types of headaches will be managed differently. Treatments could range from simple dietary adjustments to invasive procedures performed by a medical professional.
- Not everyone will respond to the same treatments, even for the same types of headaches. If you are experiencing headaches you cannot treat, speak with a doctor about a treatment plan.
- Read on to learn more about the most common treatments for each type of headache.
Tension headache
An OTC pain reliever may be all it takes to relieve your occasional headache symptoms. OTC pain relievers include:
- aspirin
- ibuprofen (Advil)
- naproxen (Aleve)
- acetaminophen and caffeine
If OTC medications are not providing relief, your doctor may recommend prescription medication, such as:
- indomethacin
- meloxicam (Mobic)
- ketorolac
When a tension headache becomes chronic, a different action may be suggested to address the underlying headache trigger.
Cluster headache
A doctor may recommend the following to provide relief for the symptoms:
- oxygen therapy
- sumatriptan (Imitrex)
- local anaesthetic (lidocaine)
After a diagnosis, your doctor will work with you to develop a prevention plan. The following may put your cluster headaches into a period of remission:
- corticosteroids
- melatonin
- topiramate (Topamax)
- calcium channel blockers
- Migraine
If OTC pain relievers do not reduce migraine pain during an attack, a doctor might prescribe triptans. Triptans are drugs that decrease inflammation and change blood flow within your brain. They come in the form of nasal sprays, pills, and injections. Popular options include:
- sumatriptan (Imitrex)
- rizatriptan (Maxalt, Axert)
Speak with a doctor about taking a daily medication to prevent migraine headaches if you experience headaches that are:
- debilitating more than three days a month
- somewhat debilitating four days a month
- lasting longer than six days a month
According to a 2019 review, preventive migraine medications are significantly underused: Only 3 to 13 per cent of those with migraine take preventative medicine, while up to 38 per cent need it.
How to prevent it:
Preventing migraine dramatically improves the quality of life and productivity.
Helpful preventive migraine medications include:
- propranolol (Inderal)
- metoprolol (Toprol)
- topiramate (Topamax)
- amitriptyline
- Hemicrania continua
One of the defining characteristics of hemicrania continua is a complete response to indomethacin, a drug in the nonsteroidal anti-inflammatory drug (NSAID) family. A low dose of three times daily with meals usually relieves symptoms within 24 hours.
Taking indomethacin can have side effects, especially at higher doses, so taking the lowest effective dose is recommended.
- Ice pick headache:
Ice pick headaches can be challenging to treat because they last for a short duration. Most ice-pick headaches are over before you can do much about them.
You might take preventive measures to reduce the frequency or intensity of future headaches. Treatments could include:
- indomethacin
- gabapentin
- cyclooxygenase-2 (COX-2) inhibitors
- melatonin
- external hand warming
- Thunderclap headache
Thunderclap headache:
If your thunderclap headache results from another condition, you will need to treat the underlying condition.
If your thunderclap headache is not caused by something else, it is a primary one. These could be treated with NSAIDs, such as indomethacin. Other treatments for thunderclap headaches include Trusted Source:
- calcium channel blockers
- beta-blockers
- topiramate
- lithium
- triptans
- Allergy or sinus headache
Sinus headaches are treated by thinning out the mucus that builds up and causes sinus pressure. Options include:
- Nasal steroid sprays
- OTC decongestants like phenylephrine (Sudafed PE)
- antihistamines like cetirizine
A sinus headache can also be a symptom of a sinus infection. In these cases, your doctor may prescribe antibiotics to clear the infection and relieve your headache and other symptoms.
Can you prevent headaches?
Many headaches can be managed with preventive measures, but the methods will differ by headache type. Some headache types might be prevented with medication, while the same drug might cause others. For this reason, it is essential to know what works for you.
Discuss preventive treatments with a doctor to find a plan that fits your needs. Headache prevention could mean reduced headache frequency or intensity or prevention of headaches altogether.
In general, many headaches can be prevented or improved with lifestyle changes, including:
- getting enough sleep on a regular schedule
- getting enough to eat and eating balanced meals
- staying hydrated
- getting adequate regular exercise
- managing stress
Migraine headaches may be prevented with calcitonin gene-related peptide (CGRP) medication. The Food and Drug Administration (FDA) has approved one CGRP medication, Emgality, to prevent cluster headaches.
Conclusion:
- Your outlook will depend on the type of headache you are having.
- Primary headaches do not cause Trusted Source permanent disability or death. However, if they are frequent and severe enough, they could be debilitating temporarily. These headache types can often be managed when adequately diagnosed and treated.
- The conclusion for secondary headaches will depend on the underlying cause. Some can be managed through simple changes to routines, while others could be fatal without immediate medical attention.
- If you are experiencing recurring or severe headaches, get medical assistance immediately. An accurate diagnosis will be the first step in understanding and managing your headaches. These are the Types of Headaches
Read More:
- Antimicrobial Stewardship School
- Sepsis Training Program
- Download Pocket Guide for Antibiotic Pharmacotherapy Book
- Microbiology Course | ABC Bacteria
- Infectious Disease E-News | FREE Subscription
- ABC antimicrobials | Know all about the Antimicrobials
- Road Map to Antimicrobial Stewardship Training Program
- Register Now at FADIC Clinical Research School
- FADIC Drug Information Fellowship
- Buy FADIC Toolkit for Writing Research to Write a Great Research Paper
- Read 10 Skills You Must Learn to Do Research via Google Scholar in Arabic
- The FADIC Online Continuous Medical Improvement Programs & Mini-Courses.
- Check Now the FADIC Book store and Buy books in different specialities.
- Watch Now FADIC TV to Keep Yourself Updated.
- FADIC Podcast focuses on varieties of pharmacist perspectives in different specialities.
- Subscribe Now to FADIC 2020 Daily News (FNN) and Keep Updated.
- Check Now about Coronavirus Resource Information Center.

 Log in
Log in Sign up
Sign up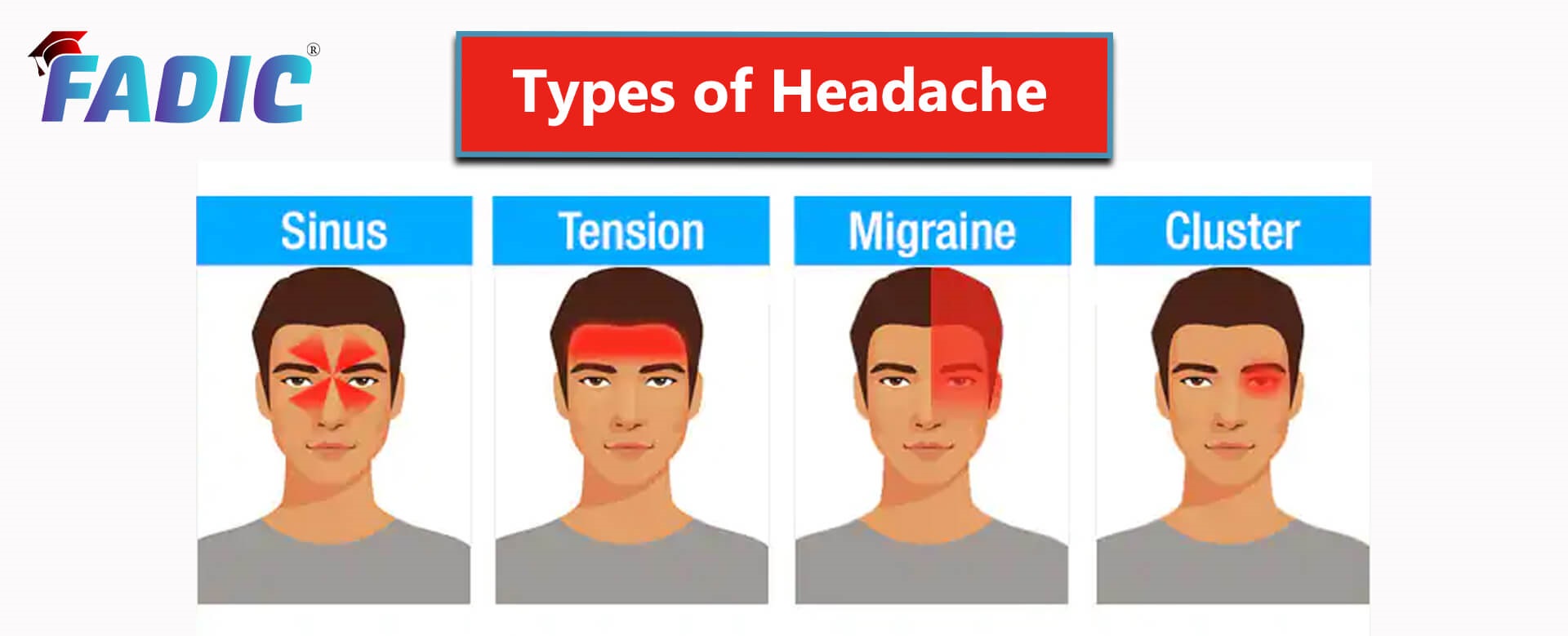 Types of Headaches
Types of Headaches
