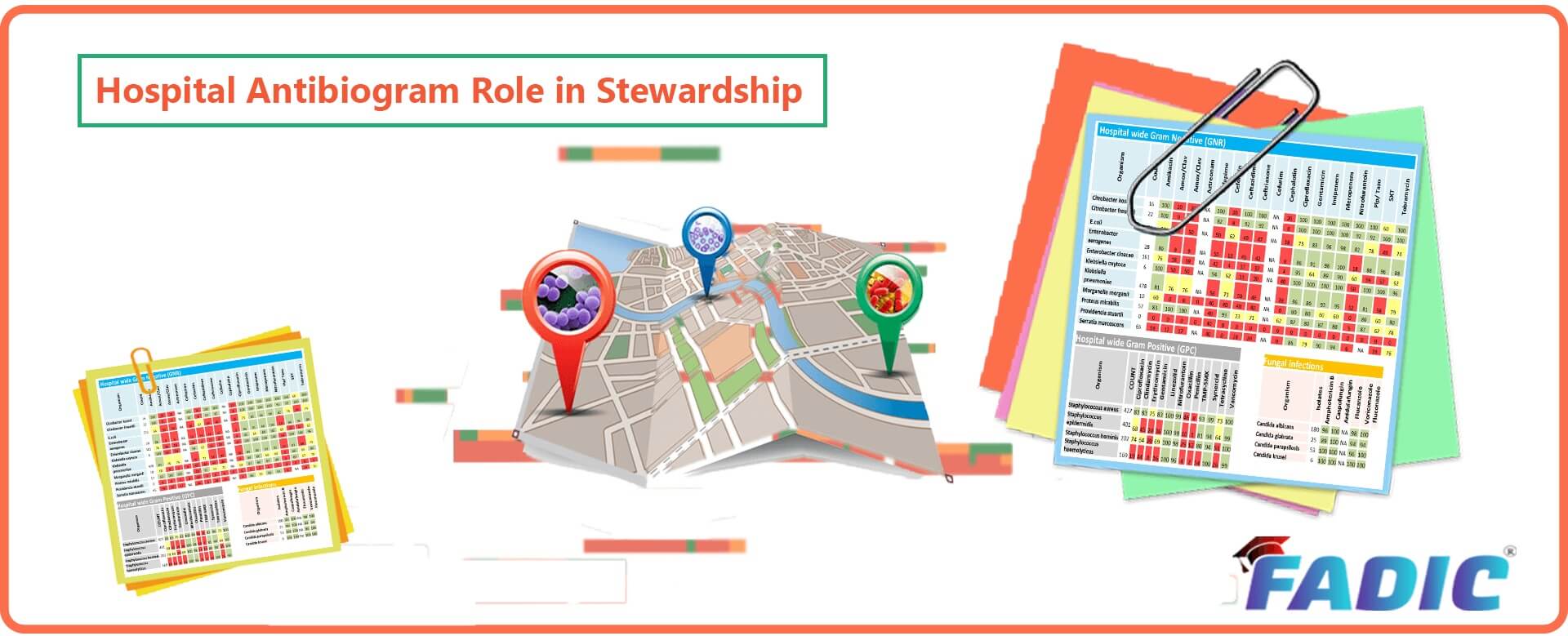
Hospital Antibiogram Role in Antimicrobial Stewardship
Hospital Antibiogram Role in Antimicrobial Stewardship
By: Rasha Abdelsalam Elshenawy
Hospital Antibiogram Definition:
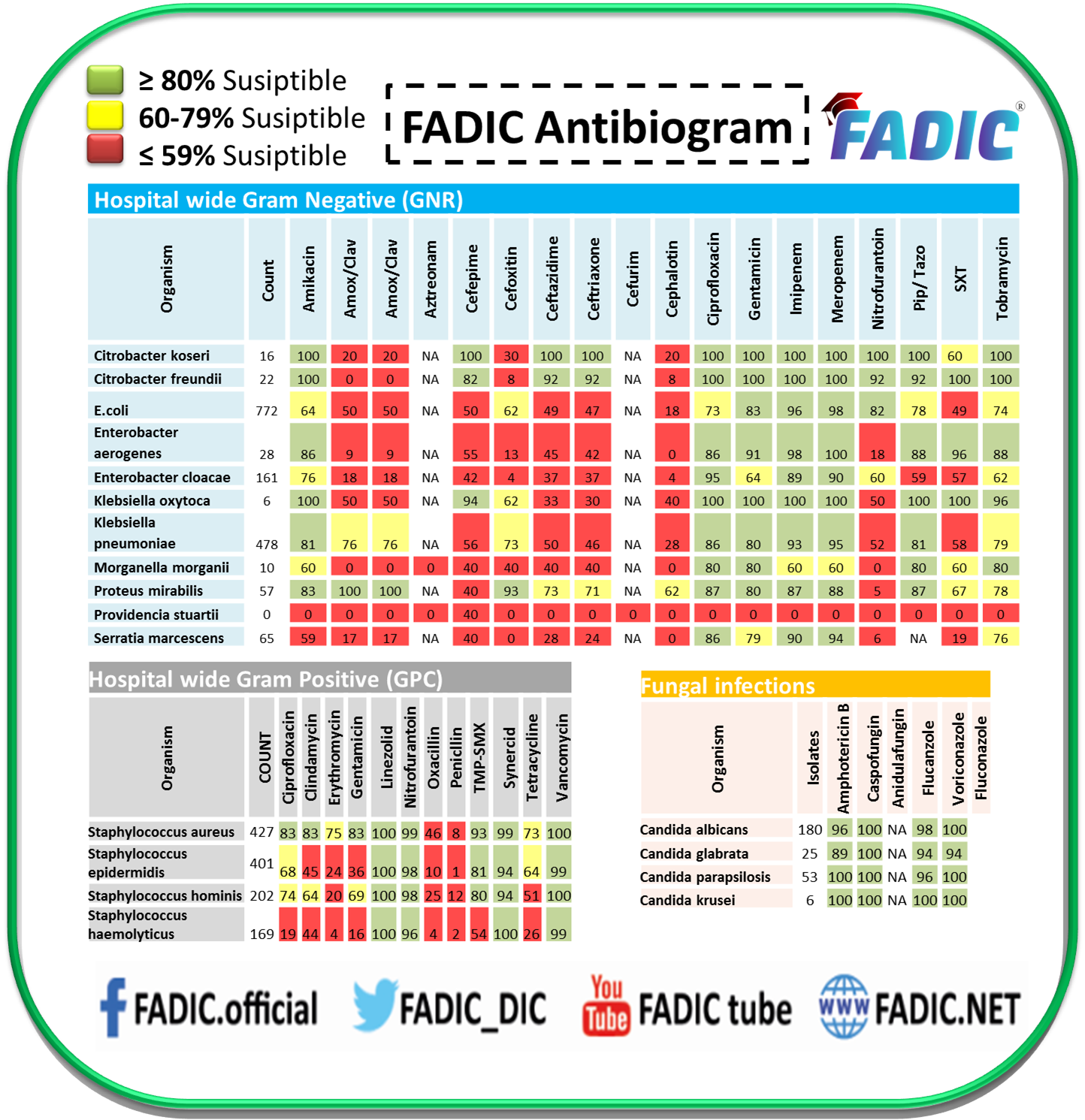
- Firstly, the antibiogram summarises the cumulative susceptibility of bacterial isolates to formulary antibiotics during a specified period.
- Additionally, it represents the proportion of each bacterium that is susceptible to a given formulary antibiotic.
Highly Recommend this Hydrossential Serum: Amazing for your Skin
How is an Antibiogram produced?
- To determine whether a specific antibiotic may be effective versus a given bacterial isolate, susceptibility testing can be performed in a microbiology laboratory.
- Moreover, if the antibiotic is found to work against the bacteria, it is labelled as “S” for susceptible.
- If the antibiotic is found not to work against the bacteria, it is labelled as “R” for resistance.
- In some instances, sensitivity testing results fall between susceptible and resistant.
- In these cases, the result may be called “I” for intermediate or “S-DD” for susceptible, dose-dependent.
- Over a year, a hospital may report hundreds or thousands of susceptibility testing results.
- This data can be combined into a cumulative report, more commonly known as a hospital antibiogram or institutional antibiogram.
- Additionally, antibiograms can vary significantly between hospitals.
- You cannot take the antibiogram from one hospital and apply it to another.
- Even hospitals in the same city located directly across the street can have antibiograms that look entirely different.
- A big reason why antibiograms differ between hospitals is that each hospital serves specific patient populations and provides unique clinical services.
- Antibiograms are an essential tool in the fight against antibiotic-resistant organisms.
- Finally, they can help identify problematic pathogens or help identify which antibiotics to give a sick patient.
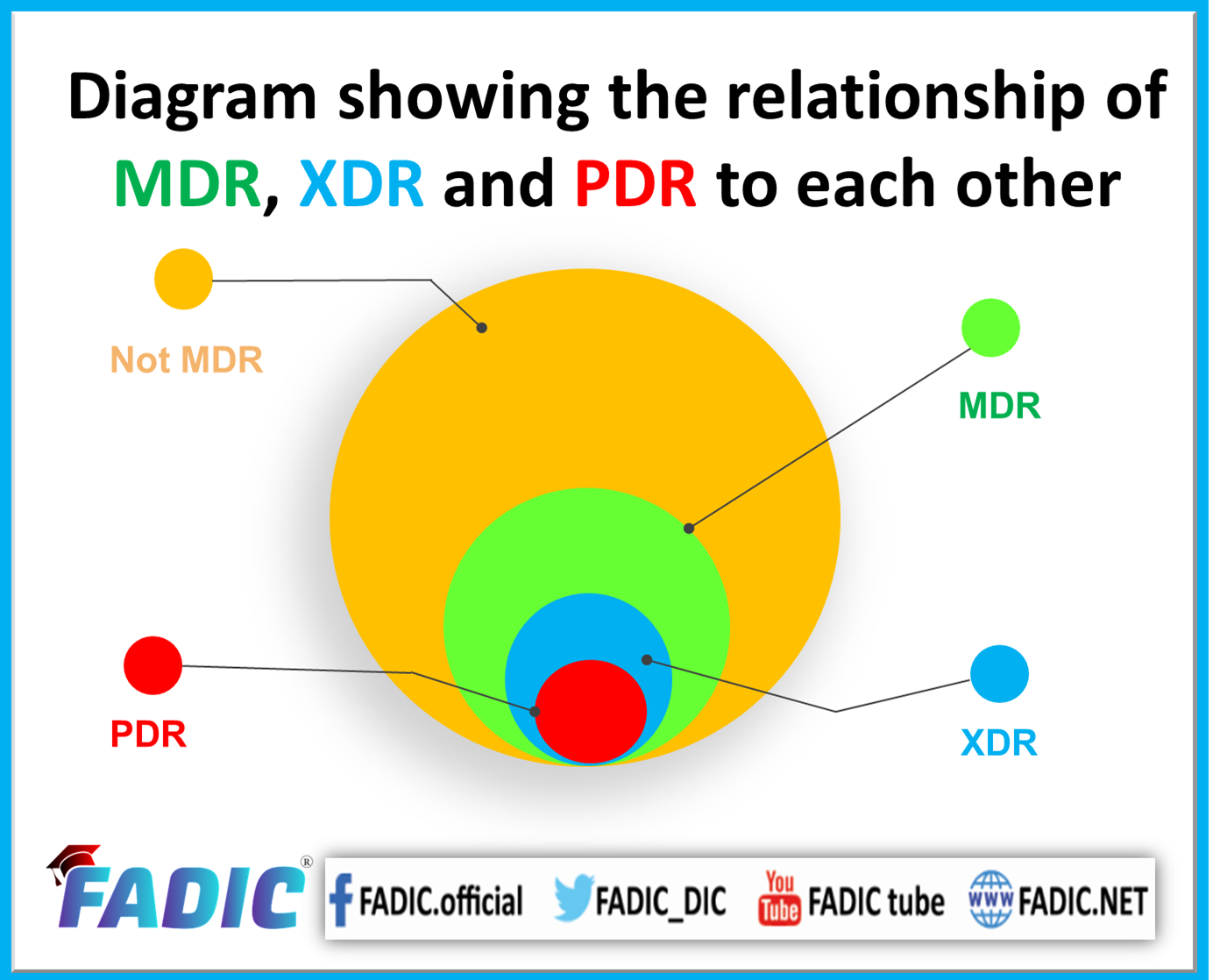
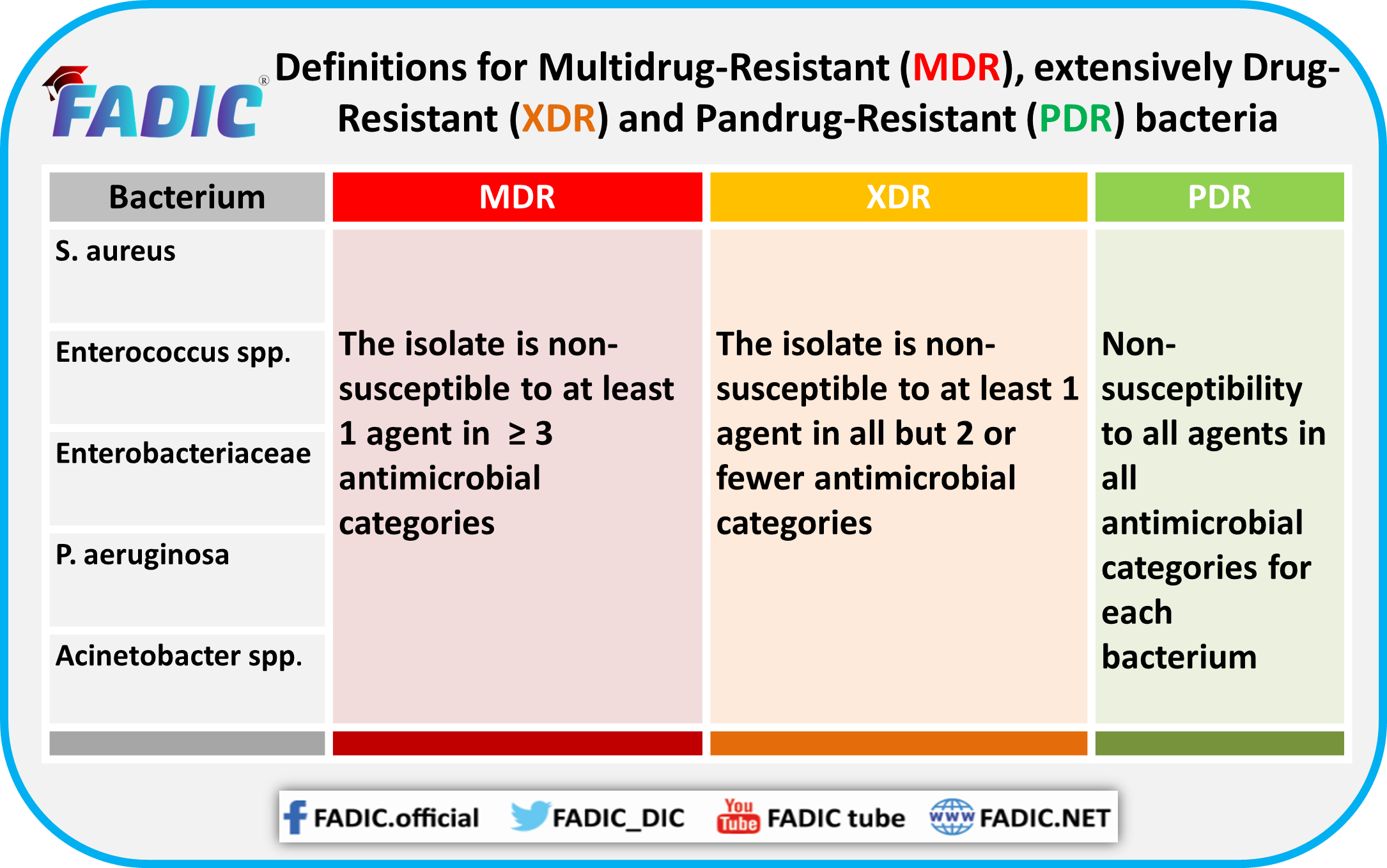
Types of Bacterial Resistance (MDR, XDR and PDR)
MDR
- Non-susceptibility to at least one agent in three or more antimicrobial categories.
- These include strains of Acinetobacter baumannii resistant to all antimicrobial agents except imipenem.
- Organisms such as Stenotrophomonas maltophilia, Burkholderia cepacia, and Ralstonia pickettii that are intrinsically resistant to the broadest-spectrum antimicrobial agents
XDR
- Firstly, non-susceptibility to at least one agent in all but two or fewer antimicrobial categories (i.e. bacterial isolates remain susceptible to only one or two categories).
- Initially, the term XDR was created to describe extensively-drug resistant Mycobacterium 24 tuberculosis (XDR MTB).
- Finally, XDR defined as “resistance to the first-line agent’s isoniazid and rifampicin, to a fluoroquinolone, and at least one of the three second-line parenteral drugs (i.e. amikacin, kanamycin or capreomycin)”.
PDR
- Additionally, the non-susceptibility to all agents in all antimicrobial categories (i.e. no agents tested as susceptible for that organism).
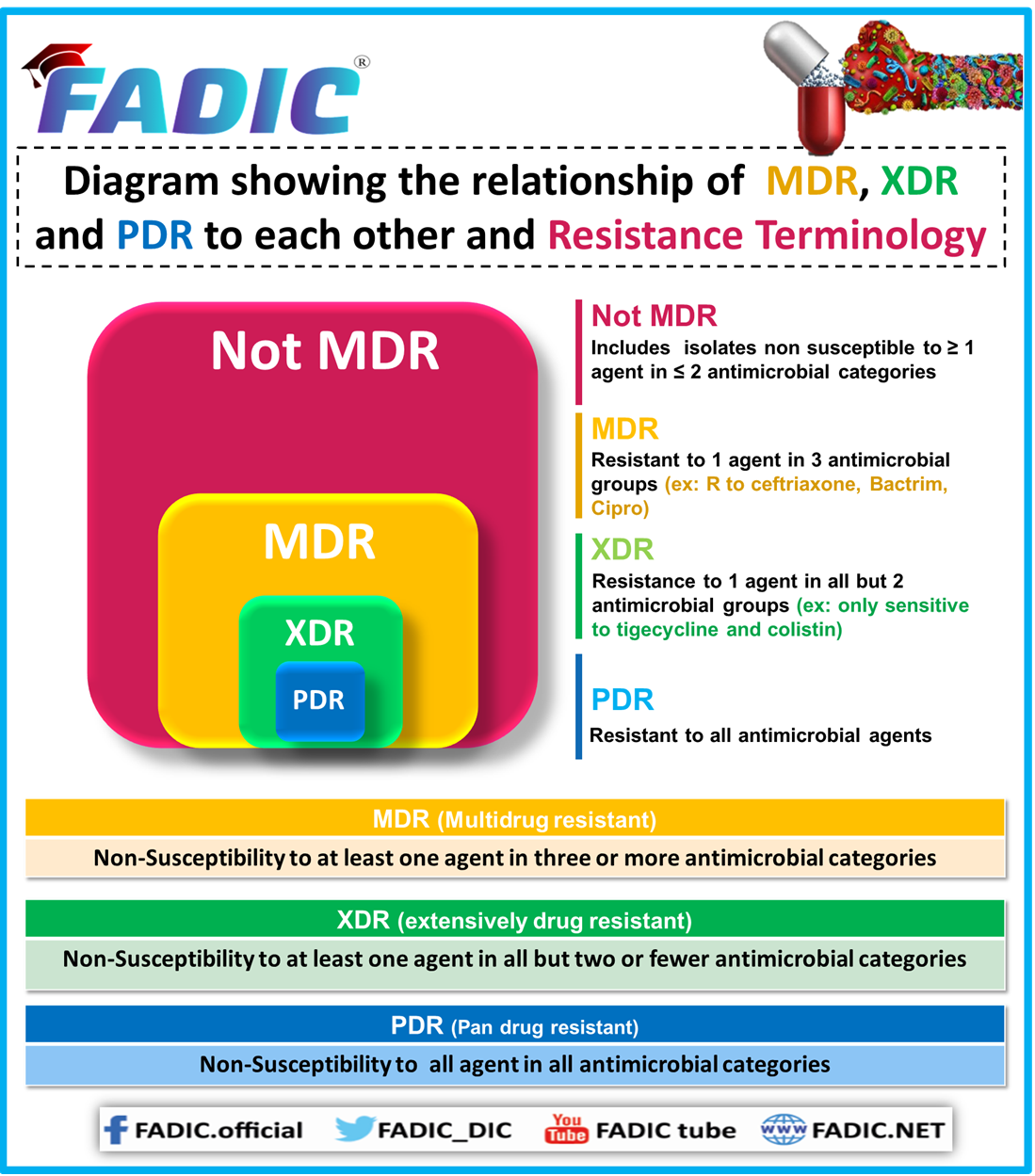
Comparison between the MDR, XDR, and PDR
Importance of Antibiogram
-
Antibiograms can help pick empiric antibiotic therapy.
- Firstly, empiric therapy is the antibiotic regimen before knowing organism identification and sensitivities.
- This therapy type is selected based on case-specific factors, which help clinicians identify the most likely organisms to cause infection in a particular patient case scenario.
- If two drugs both have a resistance rate below 20% and are both being considered for the part of empiric therapy in managing a severe infection.
- In addition, the clinician may opt to go with the antibiotic that is more likely to cover the bacteria as indicated by the local antibiogram.
-
Antibiograms help track local antibiotic resistance trends.
- Firstly, reviewing antibiogram data can help us to see the big picture.
- Moreover, having an idea of what types of antibiotic resistance to be on the lookout for at your institution can improve your ability to avoid suboptimal therapies and, in turn, provide better care.
- Finally, it may also assist in identifying the overuse of specific antibiotics, as more antibiotic use leads to more antibiotic resistance.
Advantages of Antibiogram
- The antibiogram gives clinicians information about institution-specific resistance patterns.
- Additionally, it provides them with the recommended way to track the resistance.
- Moreover, multiple uses:
- Monitoring resistance trends.
- Comparing susceptibility rates between institutions (if similar methods are used).
- Helping in formulary decision-making.
- Informing local/institutional recommendations for the selection of empiric therapy
- Identifying stewardship initiatives and targets for education
Disadvantages of Antibiogram
- Challenging for smaller institutions, those without sufficient microbiology laboratory support and those that outsource microbiology services:
- Additionally, except for the assessment of effects in a specific unit, antibiograms are not a reliable metric for the short-term effects of an antimicrobial stewardship program.
- Moreover, resistance patterns could be reflected in an antibiogram and the multifactorial nature of resistance).
- Finally, they have several limitations:
- Usually represent isolates from the community and hospital-acquired infections; they may not be a good reflection of either alone.
- The antibiogram is only useful only to guide the choice of empiric therapy at the institutional level.
- Cannot identify increasing subclinical resistance or “MIC creep.”
- Additionally, it cannot identify the incidence of multi-drug-resistant organisms; susceptibility is provided only for individual antibiotics
- Antibiogram reflecting cumulative hospital-wide data may dilute results and mask resistance trends for a particular ward or service (e.g., in the ICU or oncology wards).
- Conversely, when ICU data is included in an institution-wide antibiogram.
- The susceptibility patterns can show more resistance than if the ICU data were excluded and reported separately.
Requirements of Hospital Antibiogram Role in Antimicrobial Stewardship:
- Knowledgeable personnel from microbiology to collate and interpret raw data.
- Additionally, the individual (from microbiology or other) to summarise and present data.
- Individual to take responsibility for updating, publishing and disseminating a yearly update.
Hospital Antibiogram Role in Antimicrobial Stewardship
In conclusion, antibiogram highlight local (e.g., institutional) susceptibility data.
Additionally, an antibiogram will help establish the institution’s antimicrobial guidelines according to the susceptibility/resistance pattern.
They have to be published annually, Semi-annually, or Quarterly according to the microbiology laboratory support.
Finally, they can also reveal the frequency of isolation of certain organisms (e.g., whether there is a high prevalence of Pseudomonas aeruginosa in a region).
Related Courses
- Antimicrobial Stewardship Fellowship Program
- Antimicrobial Stewardship Program in Acute Care Setting
- Patient Education and Counseling Program
- ABC of Bacteria Course
Mini Courses /One-day Workshop:
- Goals of Antimicrobial Stewardship
- Respiratory Tract Infection: How to Apply Antimicrobial Stewardship?
- Practical Guide for Antimicrobial Stewardship Committee
- Antimicrobials Pharmacokinetic & Pharmacodynamic
- Clostridioides Difficile Infection (CDI) Prevention Program
- Acute Bacterial Skin and Skin Structure Infections
- Sepsis Training Program
- Antifungal Stewardship: Implementation Guide
- Antibiogram Best Use & Interpretation
- Urinalysis Tract Infection: Role of Antimicrobial Stewardship
- Surgical Prophylaxis Antimicrobial Stewardship
Books:
- Pocket Guide for Antibiotic Pharmacotherapy
- Antibiotic Cards
- FADIC Outpatient Parenteral Antimicrobial Therapy (OPAT)
- كتيب فادك للتوعية بمخاطر سوء الاستخدام للمضادات الحيوية
Keep Learning From FADIC Blog:
- Candidate Success Story – FADIC Antimicrobial Stewardship Program
- Antimicrobial Stewardship in Surgical Prophylaxis
- Hospital Antibiogram Role in Antimicrobial Stewardship
- Antimicrobial Stewardship Strategies
- Colistin Between Nebulizer and Intravenous Forms
- CDC Core elements of Antimicrobial Stewardship
- إرشادات المضادات الحيوية – لا تساوم البكتيريا تقاوم
- المضادات الحيوية الأكثر شيوعاً واستخداما في الوصفات الطبية
- المضادات الحيوية

 Log in
Log in Sign up
Sign up